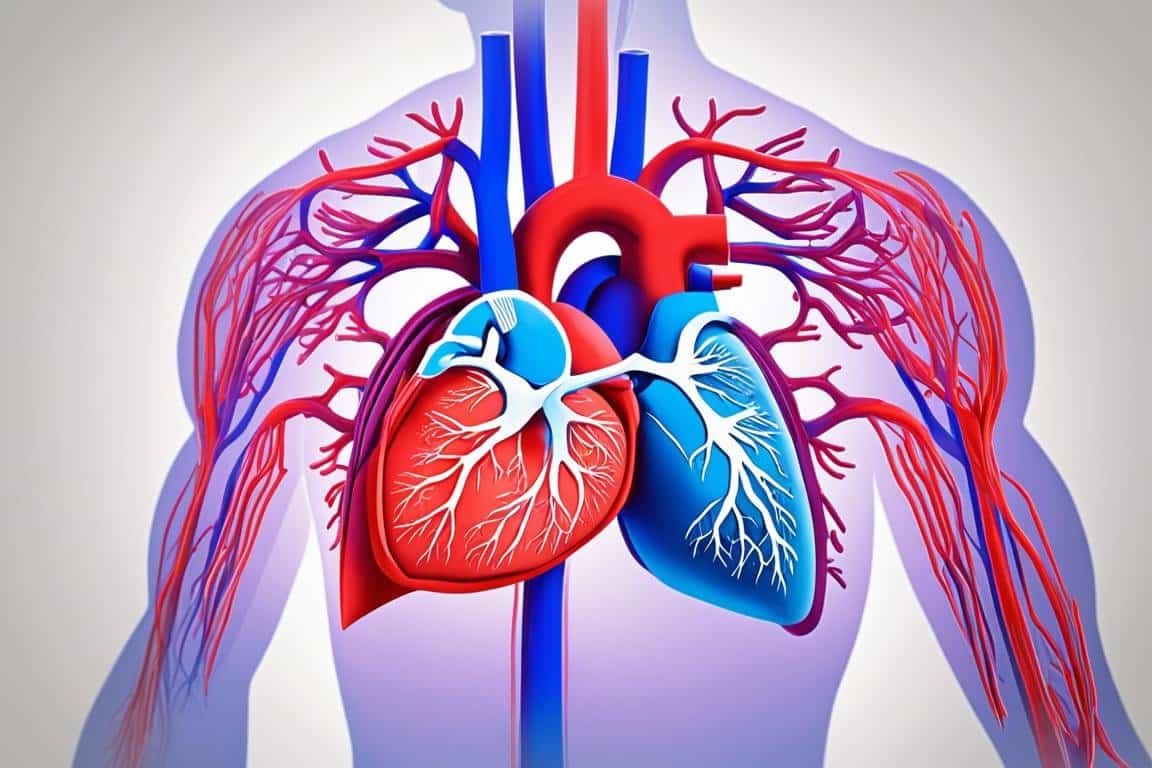
Pericarditis and myocarditis are two inflammatory conditions that can affect the heart. It is important to understand the basics of these conditions, including their definition, in order to recognize symptoms and seek appropriate treatment. Pericarditis refers to the inflammation of the pericardium, the sac that surrounds the heart. On the other hand, myocarditis is inflammation of the heart muscle itself, known as the myocardium. Both conditions can cause chest pain, fever, and have an impact on heart health.
Key Takeaways:
- Pericarditis is inflammation of the pericardium, the sac that surrounds the heart.
- Myocarditis is inflammation of the heart muscle (myocardium).
- Both conditions can cause chest pain, fever, and impact heart health.
- Recognizing symptoms and seeking appropriate treatment is crucial for managing these conditions.
- Early diagnosis and treatment can help prevent complications and promote overall heart well-being.
Causes and Risk Factors
Pericarditis, the inflammation of the pericardium, can have various causes. It can be triggered by viral infections, such as the common cold or the flu, as well as autoimmune diseases like systemic lupus erythematosus and rheumatoid arthritis. Additionally, certain drugs and toxins can also lead to pericarditis.
When it comes to viral infections, the viruses can directly infect the pericardium, causing inflammation. Autoimmune diseases, on the other hand, occur when the body’s immune system mistakenly attacks the pericardium, resulting in inflammation. As for drugs and toxins, they can cause pericarditis by directly irritating the pericardium.
Recognizing the causes and risk factors for pericarditis is crucial for understanding why it occurs and taking necessary precautions. Identifying viral infections, managing autoimmune diseases, and minimizing exposure to certain drugs and toxins can help reduce your risk of developing pericarditis.
Causes of Pericarditis
- Viral infections, such as the common cold and the flu
- Autoimmune diseases, including systemic lupus erythematosus and rheumatoid arthritis
- Medications and toxins
By understanding the causes and risk factors associated with pericarditis, you can take proactive steps to protect your heart health and prevent this inflammatory condition.
Symptoms and Diagnosis
If you suspect you may be experiencing pericarditis, it’s important to be aware of the common symptoms. The most prevalent symptom is chest pain, which is frequently aggravated when taking deep breaths. This chest pain can often radiate to the neck, shoulder, or back. In addition to chest pain, you may also experience fever and feel fatigued.
To diagnose pericarditis, your doctor will perform a thorough evaluation of your symptoms and conduct a physical examination. They may listen for a friction rub during the examination, which is a specific sound caused by the inflamed layers of the pericardium rubbing against each other. To further investigate, they may recommend additional tests such as an echocardiogram and blood tests.
An echocardiogram uses sound waves to create detailed images of your heart. This non-invasive test allows your doctor to visualize the structure and function of your heart. By examining the echocardiogram, they can look for any abnormalities or signs of inflammation that may indicate pericarditis. Additionally, blood tests help identify markers of inflammation that can assist in confirming the diagnosis.

| Symptoms of Pericarditis | Diagnostic Tests |
|---|---|
|
|
Treatment Options
When it comes to treating pericarditis, the primary goals are to alleviate pain and reduce inflammation. Fortunately, there are effective treatment options available that can help you recover and restore your heart health.
Anti-inflammatory medications: The cornerstone of pericarditis treatment involves the use of anti-inflammatory medications. Nonsteroidal Anti-Inflammatory Drugs (NSAIDs), such as ibuprofen or aspirin, are commonly prescribed to reduce inflammation and relieve pain. These medications can help alleviate your symptoms and promote a faster recovery.
Colchicine: Another medication that is often used in the treatment of pericarditis is colchicine. Colchicine is an anti-inflammatory drug that can help prevent recurrent episodes of pericarditis. It works by reducing inflammation and suppressing the immune response in the pericardium.
In severe or recurrent cases of pericarditis, steroids may be recommended. Steroids are potent anti-inflammatory medications that can effectively alleviate symptoms and reduce inflammation. However, they are typically used as a last resort due to potential side effects.
The specific treatment plan for pericarditis will depend on the underlying cause of the condition and your individual needs. It’s important to work closely with your healthcare provider to determine the most appropriate treatment approach for you.
Complications and Prognosis
While most cases of pericarditis resolve without complications, it’s important to be aware of potential risks that can arise. Two serious complications associated with pericarditis are constrictive pericarditis and cardiac tamponade.
Constrictive pericarditis: This condition occurs when the pericardium, the sac surrounding the heart, becomes thickened and stiff. As a result, the heart is restricted in its ability to fill properly, leading to decreased cardiac output. Common causes of constrictive pericarditis include chronic inflammation, infection, or prior pericardial surgery. If left untreated, constrictive pericarditis can significantly affect heart function and lead to symptoms such as fatigue, edema, and shortness of breath.
Cardiac tamponade: Cardiac tamponade is a life-threatening condition that occurs when fluid accumulates within the pericardial sac, putting pressure on the heart and impeding its ability to pump blood effectively. This can happen as a result of acute pericarditis, trauma, or other medical conditions. Symptoms of cardiac tamponade include chest pain, low blood pressure, shortness of breath, and fainting. Immediate medical intervention is necessary to relieve the fluid buildup and restore normal heart function.
It is crucial to seek prompt medical attention if you experience any symptoms of constrictive pericarditis or cardiac tamponade. Early diagnosis and appropriate treatment can help prevent these complications and improve the prognosis. Your healthcare provider may recommend imaging tests, such as an echocardiogram or cardiac MRI, to assess the condition of your pericardium and determine the best course of action.

| Complications | Constrictive Pericarditis | Cardiac Tamponade |
|---|---|---|
| Definition | Thickening and stiffness of the pericardium restricting heart filling | Fluid accumulation within the pericardial sac compressing the heart |
| Causes | Chronic inflammation, infection, prior pericardial surgery | Acute pericarditis, trauma, other medical conditions |
| Symptoms | Fatigue, edema, shortness of breath | Chest pain, low blood pressure, shortness of breath, fainting |
| Treatment | Medication, pericardiectomy | Emergency fluid removal, pericardiocentesis |
Understanding Myocarditis
Myocarditis is a condition characterized by inflammation of the heart muscle, known as the myocardium. It can be caused by various factors including viral infections, bacterial infections, or autoimmune diseases.
Symptoms of myocarditis can vary depending on the severity of inflammation and individual factors. Common symptoms may include:
- Chest pain: This is a common symptom of myocarditis and may be experienced as a dull ache or sharp pain in the chest.
- Fatigue: Feeling excessively tired or having decreased energy levels.
- Shortness of breath: Difficulty breathing or feeling breathless even during minimal physical activity.
Diagnosing myocarditis involves a comprehensive approach to evaluate the patient’s medical history, perform a physical examination, and conduct diagnostic tests. These tests may include:
- Blood tests: These tests help identify markers of inflammation in the body and can aid in diagnosing myocarditis.
- Electrocardiogram (ECG): An ECG measures the electrical activity of the heart and can detect abnormalities that may indicate myocarditis.
- Cardiac imaging: These tests, such as echocardiography or cardiac MRI, provide visual images of the heart to assess its structure and function.
Proper diagnosis and early detection of myocarditis are crucial for developing an effective treatment plan and preventing potential complications. Prompt medical attention should be sought if you experience any symptoms associated with myocarditis to ensure appropriate management of the condition.
| Causes | Symptoms | Diagnosis |
|---|---|---|
|
|
|
Conclusion
Pericarditis and myocarditis are inflammatory conditions that can have a significant impact on heart health. Understanding the basics of these conditions, including their causes, symptoms, diagnosis, and treatment options, is crucial for maintaining a healthy heart.
If you experience symptoms such as chest pain, fever, or shortness of breath, it is essential to seek immediate medical attention for a proper diagnosis and appropriate treatment. Prompt intervention can help prevent further complications and promote overall heart well-being.
Managing pericarditis and myocarditis requires proactive steps, such as adhering to prescribed treatments, making necessary lifestyle changes, and attending regular follow-up appointments with your healthcare provider. By taking control of your heart health and following recommended guidelines, you can reduce the risk of complications and lead a fulfilling life.