
Introduction
Have you ever wondered what exactly happens during a heart attack? 🤔 Like a river blocked by a dam, a heart attack occurs when blood flow to the heart is obstructed, leading to serious consequences. This blog is your guide to understanding the science and pathology behind heart attacks, tailored for busy Indian professionals in their 30s, 40s, and 50s.
In simple terms, we’ll explore how a heart attack, or myocardial infarction, happens. It’s often caused by a buildup of substances like fat and cholesterol in the coronary arteries, leading to a severe reduction or complete blockage of blood flow to the heart. 🚑 Recognizing the symptoms is vital for timely treatment, which can range from chest pain to more subtle signs like fatigue and shortness of breath.
We’ll also discuss the various causes of heart attacks, from coronary artery disease to other less common factors. Plus, we’ll delve into the risk factors, such as ageing, tobacco use, high blood pressure, and more, providing you with the knowledge to take proactive steps towards prevention and recovery. 🌱
Whether you’re seeking to understand this critical health issue better or looking for ways to protect your heart, this blog is your friendly and motivating companion. Let’s embark on this journey to heart health together! ❤️
Unblocking Life: Part 1
In the bustling city of Mumbai, where the streets echoed with life, lived Amit, a 46-year-old advertising executive. His life was a canvas of campaigns and deadlines, always moving at a breakneck pace.
Amit, a father of two, was the picture of success. But his lifestyle was a silent adversary. Long hours at the desk, fast food, and negligible exercise were his norm. His wife often warned him about his health, but Amit shrugged it off, lost in the demands of his career.
Causes of Heart Attacks
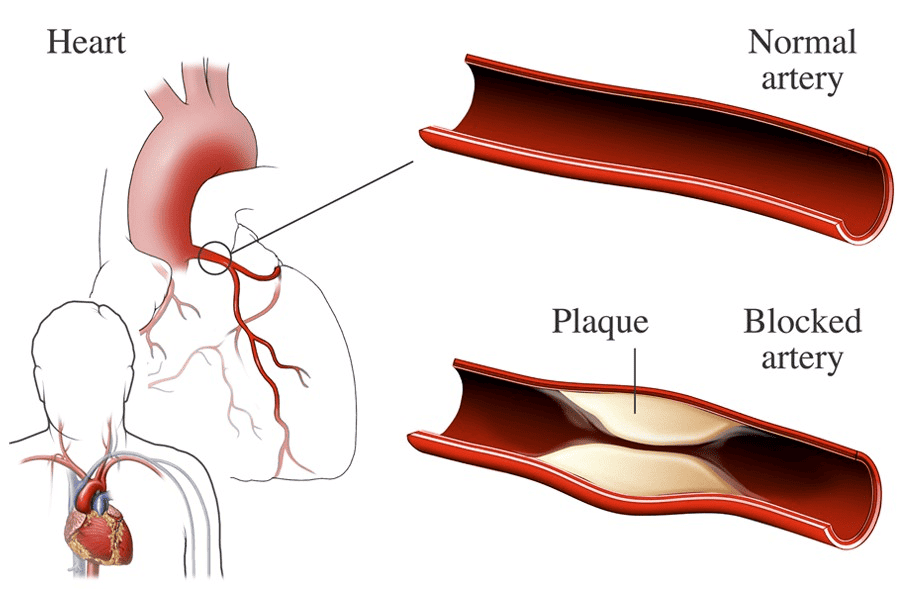
Normal versus a blocked artery
Photo Credit: https://www.nhlbi.nih.gov/health/coronary-heart-disease/causes
Coronary artery disease is the primary cause of most heart attacks. It occurs when the coronary arteries, which supply blood to the heart, become narrow due to the buildup of plaque. When plaque buildup ruptures, it can cause a complete or partial blockage of the arteries, leading to a heart attack.
Plaque is made up of fat, cholesterol, and other substances that accumulate on the artery walls. Over time, this plaque buildup can reduce blood flow to the heart, causing the heart muscle to receive less oxygen and nutrients. In some cases, a piece of the plaque can break off, forming a blood clot that completely blocks the artery.
“Coronary artery disease is the leading cause of heart attacks, resulting from the narrowing of the coronary arteries due to plaque buildup.”
In addition to coronary artery disease, there are other causes of heart attacks. These include:
- Coronary Artery Spasm: Spasms in the coronary arteries can restrict blood flow to the heart, leading to a heart attack.
- Certain Infections: Infections such as COVID-19 can cause inflammation and damage to the blood vessels, increasing the risk of a heart attack.
- Spontaneous Coronary Artery Dissection (SCAD): SCAD is a rare condition where a tear occurs in the layers of the coronary artery wall, leading to a blockage and potentially causing a heart attack.
Simple Flowchart describing the mechanism a of Heart Attack
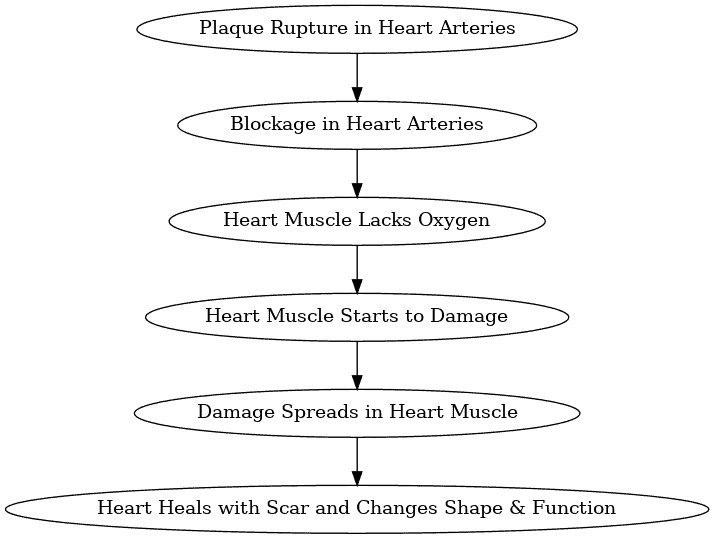
Source Link: https://www.ncbi.nlm.nih.gov/books/NBK537076/
Understanding the causes of heart attacks can help individuals take preventive measures and seek timely medical attention to reduce the risk of experiencing a heart attack.
| Cause | Description |
| Coronary Artery Disease | Narrowing of the coronary arteries due to plaque buildup |
| Coronary Artery Spasm | Spasms in the coronary arteries restricting blood flow to the heart |
| Certain Infections | Infections causing inflammation and damage to blood vessels |
| Spontaneous Coronary Artery Dissection (SCAD) | Tearing of the coronary artery wall, leading to a blockage |
Heart Attack Risk Factors
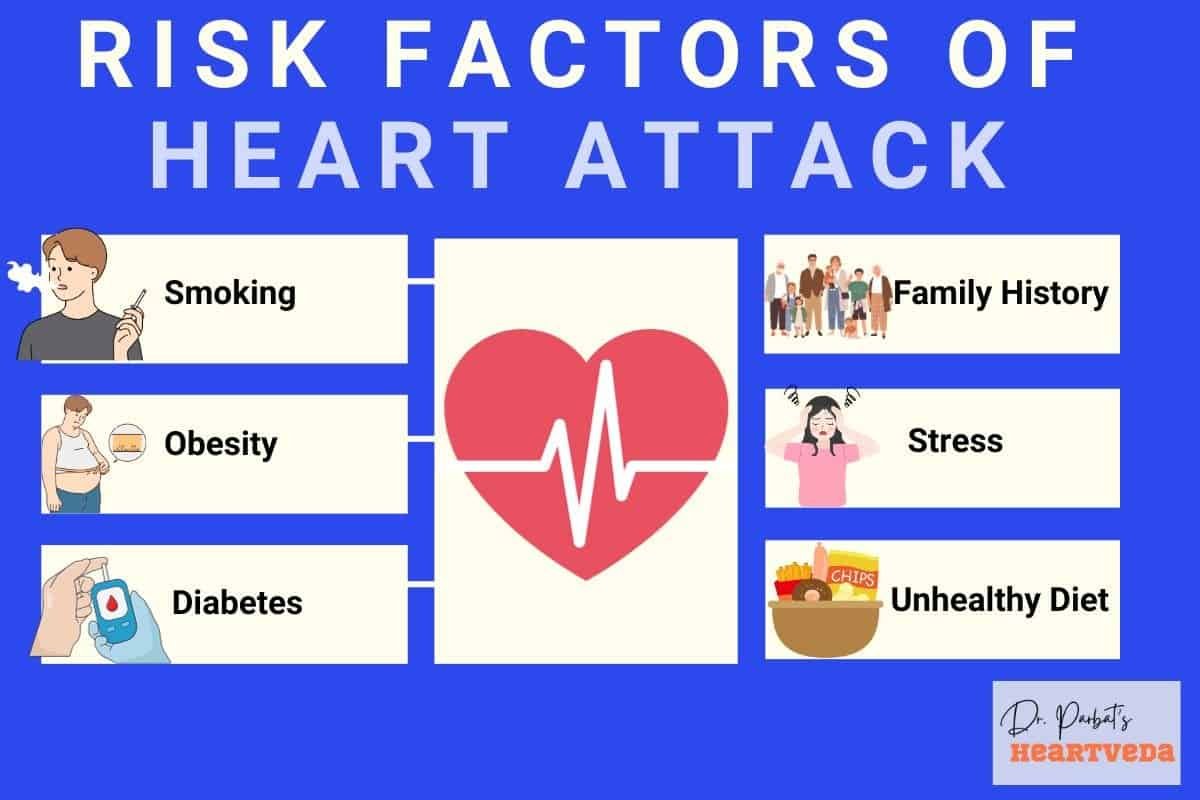
Several factors increase the risk of having a heart attack. By understanding and managing these risk factors, you can take proactive steps to prevent heart attacks and promote heart health.
Aging
As you age, your risk of heart attacks increases. The risk tends to be higher for men aged 45 and older, and women aged 55 and older.
Tobacco Use
Smoking and using tobacco products significantly raise the risk of heart attacks. The harmful chemicals in tobacco can damage your heart and blood vessels, leading to plaque buildup, a significant risk factor for a heart attack.
High Blood Pressure
Having high blood pressure puts extra strain on the heart and blood vessels, increasing the risk of heart attacks. Regular monitoring and management of blood pressure are essential.
High Cholesterol
Elevated levels of cholesterol, particularly LDL (bad) cholesterol, can contribute to the development of plaque in the arteries, narrowing the blood vessels and increasing the risk of heart attacks.
Obesity
Being overweight or obese puts extra strain on the heart and can contribute to the development of other risk factors like high blood pressure and diabetes, further increasing the risk of heart attacks.
Diabetes
Diabetes increases the risk of heart attacks due to its impact on blood sugar levels and blood vessel health. The management of diabetes is critical in reducing the risk of heart attacks.
Stress
Chronic stress can contribute to the development of unhealthy habits such as overeating, smoking, and excessive alcohol consumption, all of which can increase the risk of heart attacks.
Family History
If you have a close relative who has experienced a heart attack, your own risk of heart attacks may be higher. Genetic factors and shared environmental influences play a role in this increased risk.
Lack of Exercise
A sedentary lifestyle with little to no physical activity can lead to weight gain, high blood pressure, high cholesterol, and other risk factors for heart attacks can increase the risk of plaque buildup and subsequent heart attacks.. Regular exercise is crucial for heart health.
Unhealthy Diet
A diet that is high in saturated and trans fats, cholesterol, sodium, and added sugars contributes to the development of risk factors like high cholesterol, high blood pressure, and obesity, increasing the risk of heart attacks.
Illegal Drug Use
Using illegal drugs, such as cocaine or amphetamines, can temporarily narrow the blood vessels, increase blood pressure, and elevate the risk of heart attacks.
Preeclampsia
Women who have experienced preeclampsia during pregnancy have a higher risk of developing heart disease, including heart attacks, later in life. Regular monitoring and management of cardiovascular health are crucial for these women.
Autoimmune Conditions
Autoimmune conditions like rheumatoid arthritis or lupus can increase the risk of heart attacks due to the inflammation they cause in the body, affecting blood vessels and overall cardiovascular health.
By addressing these risk factors through lifestyle changes, such as quitting smoking, adopting a healthy diet, exercising regularly, managing stress, and following medical advice for other health conditions, you can significantly reduce your risk of experiencing a heart attack.
Unblocking Life: Part 2
One day, while presenting to a major client, Amit felt an unusual heaviness in his chest. He tried to ignore it, but the pain intensified, gripping him with an unrelenting force. It was a heart attack, the result of years of neglected health and clogged arteries.
Rushed to the hospital, Amit faced the harsh reality from Dr. Ishaa, a cardiologist. “Your heart was starved of oxygen due to blocked arteries. It’s a miracle you survived,” she said sternly.
Symptoms and Warning Signs of Heart Attacks
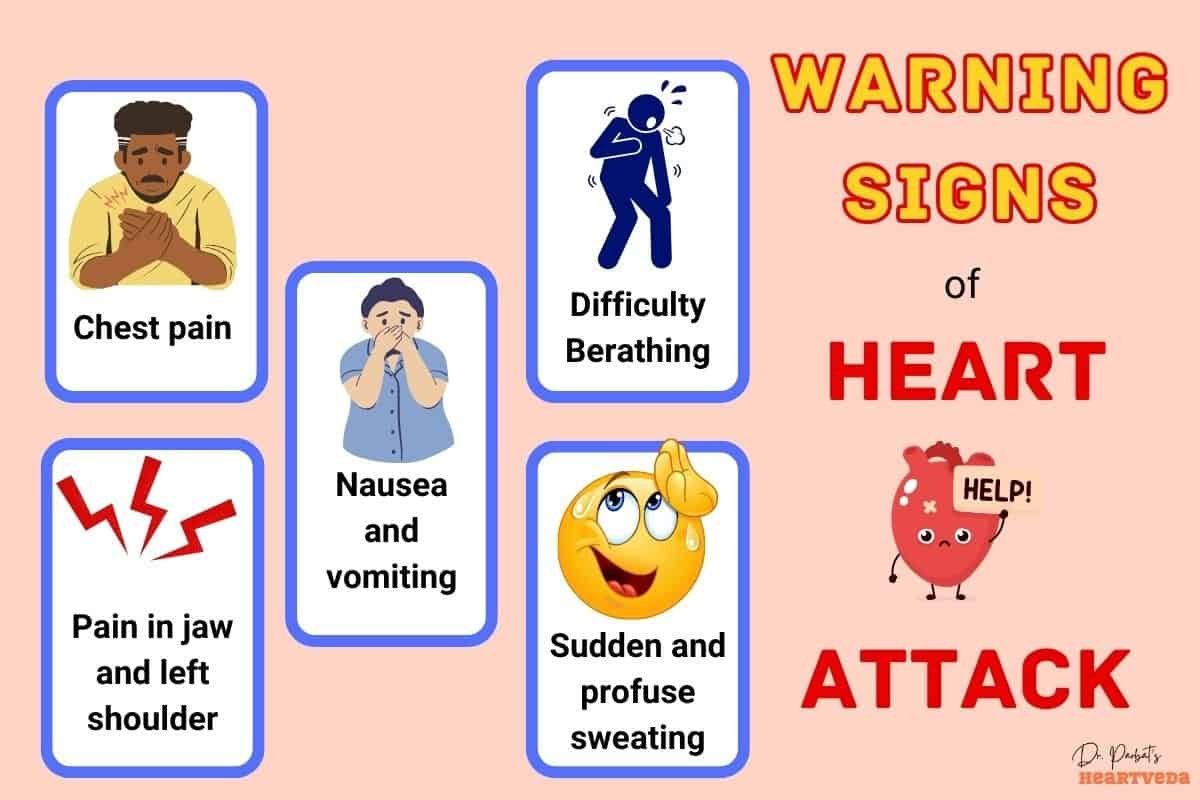
Recognizing the symptoms and warning signs of a heart attack is crucial for prompt medical intervention. While symptoms can vary, there are common signs to watch out for:
- Chest pain: This is the most common symptom of a heart attack. It may feel like pressure, tightness, or discomfort in the chest. The pain may also radiate to the shoulder, arm, back, neck, jaw, or belly.
- Spreading pain: The pain or discomfort may spread to other areas of the upper body, including the shoulder, arm, back, neck, jaw, or belly.
- Cold sweat: A sudden onset of cold sweat, often described as a clammy feeling, may occur during a heart attack.
- Fatigue: Unexplained fatigue or exhaustion is another possible symptom of a heart attack.
- Heartburn: Some people may mistake the symptoms of a heart attack for heartburn or indigestion.
- Lightheadedness: Feeling lightheaded or experiencing sudden dizziness can be a warning sign of a heart attack.
- Nausea: Nausea or a feeling of sickness in the stomach can be present during a heart attack.
- Shortness of breath: Difficulty breathing or shortness of breath may occur as the heart struggles to pump blood effectively.
- Atypical symptoms: It’s important to note that women may experience atypical symptoms such as sharp pain in the neck, arm, or back.
It’s crucial to remember that some heart attacks have warning signs and symptoms in the hours, days, or weeks leading up to the event. Recognizing and seeking medical attention for these symptoms is vital for early intervention and improved outcomes.
| Symptom | Description |
| Chest pain | Pressure, tightness, or discomfort in the chest that may spread to other areas of the upper body. |
| Spreading pain | Pain or discomfort that radiates to the shoulder, arm, back, neck, jaw, or belly. |
| Cold sweat | Sudden onset of clammy, cold sweat. |
| Fatigue | Unexplained exhaustion or fatigue. |
| Heartburn | Symptoms often mistaken for heartburn or indigestion. |
| Lightheadedness | Feeling lightheaded or experiencing sudden dizziness. |
| Nausea | Feeling of sickness or nausea in the stomach. |
| Shortness of breath | Difficulty breathing or a sensation of not getting enough air. |
| Atypical symptoms | Women may experience atypical symptoms, such as sharp pain in the neck, arm, or back. |
Unblocking Life: Part 3
The recovery was tough. Amit had to confront the truth about his lifestyle. With Dr. Ishaa’s guidance, he learned about the importance of a balanced diet, regular exercise, and stress management in keeping his heart healthy.
Determined to change, Amit embarked on a journey of transformation. He swapped junk food for heart-healthy meals, took up morning walks, and practiced yoga for stress relief. His family supported him every step of the way, delighted by his commitment.
Immediate Treatment for Heart Attacks
If you or someone else is experiencing symptoms of a heart attack, it’s crucial to call for emergency medical help immediately. Time is of the essence in saving a life during a heart attack. Delaying medical assistance can lead to severe complications or even death.
In the meantime, there are a few immediate steps you can take while waiting for medical professionals to arrive. If you have been prescribed nitroglycerin for your heart condition, take it as directed by your healthcare provider. Nitroglycerin helps relax and widen the blood vessels, improving blood flow to the heart.
Similarly, if recommended by your doctor, taking aspirin during a heart attack can be beneficial. Aspirin helps to prevent further blood clot formation by thinning the blood. However, it is essential to note that only take aspirin if your doctor has specifically advised you to do so.
In addition to medication, learning CPR (Cardiopulmonary Resuscitation) can prove to be a valuable skill to have if someone experiences a cardiac arrest during a heart attack. Performing CPR on a person in cardiac arrest can help maintain blood flow and oxygen supply until professional medical help arrives.
Remember, it is critical to prioritize your safety by immediately seeking professional medical assistance in the event of a heart attack. Calling for emergency help, taking prescribed medication as directed, if applicable, and knowing how to perform CPR can make a significant difference in saving a life.
Complications of Heart Attacks
A heart attack can have various complications that pose serious risks to your health. Understanding these complications is crucial in recognizing their signs and seeking immediate medical attention for proper treatment and management. The following are some of the common complications associated with heart attacks:
1. Irregular Heart Rhythms (Arrhythmias)
During a heart attack, the electrical impulses in your heart may be disrupted, leading to abnormal heart rhythms or arrhythmias. These irregular rhythms can cause your heart to beat too fast, too slow, or irregularly. Arrhythmias can be life-threatening and require immediate medical intervention to restore normal heart rhythm.
2. Cardiogenic Shock
If a heart attack is severe and extensive, it can cause significant damage to the heart muscle, compromising its ability to pump blood effectively. This condition, known as cardiogenic shock, occurs when the heart cannot supply enough blood and oxygen to meet the body’s needs. Cardiogenic shock is a medical emergency that requires immediate treatment to stabilize the patient’s condition.
3. Heart Failure
Heart failure, also known as congestive heart failure, can develop as a long-term complication of a heart attack. It occurs when the heart muscle is weakened and cannot pump blood efficiently to meet the body’s demands. Heart failure can cause symptoms such as shortness of breath, fatigue, and fluid retention. Proper management and treatment are essential for improving heart function and quality of life.
4. Pericarditis
Pericarditis is the inflammation of the pericardium, the thin sac-like membrane that surrounds the heart. It can occur as a result of the heart attack itself or as a complication of the healing process. Pericarditis can cause chest pain, fever, and other flu-like symptoms. Treatment aims to reduce inflammation and relieve symptoms.
5. Cardiac Arrest
Cardiac arrest is a sudden and abrupt cessation of the heart’s pumping function. It can occur as a complication of a heart attack when the electrical system of the heart malfunctions, causing the heart to stop beating altogether. Cardiac arrest is a life-threatening emergency that requires immediate cardiopulmonary resuscitation (CPR) and defibrillation to restore a normal heart rhythm.
These complications emphasize the importance of prompt medical attention and proper management after a heart attack. It is crucial to recognize the signs and symptoms of these complications and seek immediate medical help to improve outcomes and prevent further damage to the heart.
| Complication | Description |
| Irregular Heart Rhythms (Arrhythmias) | Disruption of electrical impulses in the heart, causing abnormal heart rhythms. |
| Cardiogenic Shock | Damaged heart muscle leading to inadequate blood supply and oxygen to the body. |
| Heart Failure | Weakness in the heart muscle, resulting in the ineffective pumping of blood. |
| Pericarditis | Inflammation of the thin sac-like membrane surrounding the heart. |
| Cardiac Arrest | Sudden cessation of the heart’s pumping function. |
Prevention of Heart Attacks
To reduce the risk of heart attacks, it is important to adopt a healthy lifestyle and take proactive steps to manage other health conditions. By following these recommendations, you can significantly improve your heart health:
Avoid Smoking
Smoking is a major risk factor for heart disease. Quitting smoking is one of the best things you can do to protect your heart. Seek support from healthcare professionals, join smoking cessation programs, and use nicotine replacement therapies if necessary.
Maintain a Healthy Weight
Being overweight or obese increases the strain on your heart and raises the risk of heart disease. Maintain a balanced diet and engage in regular physical activity to maintain a healthy weight.
Exercise Regularly
Regular exercise strengthens your heart and improves overall cardiovascular health. Aim for at least 150 minutes of moderate-intensity aerobic activity or 75 minutes of vigorous-intensity activity every week.
Eat a Balanced Diet
Follow a diet rich in fruits, vegetables, whole grains, lean proteins, and healthy fats. Limit saturated and trans fats, cholesterol, sodium, and added sugars. Consult a registered dietitian for personalized dietary recommendations.
Manage Stress
Chronic stress can contribute to heart disease. Find healthy ways to manage stress, such as practicing relaxation techniques, engaging in hobbies, connecting with loved ones, and seeking professional help if needed.
Manage Other Health Conditions
If you have conditions like high blood pressure, high cholesterol, or diabetes, it is essential to effectively manage them through lifestyle changes and appropriate medication. Regularly monitor your health and follow your healthcare provider’s recommendations.
By adopting a healthy lifestyle and effectively managing your health, you can greatly reduce the risk of heart attacks. Remember, small changes can make a big difference in your heart health.
Recovery from a Heart Attack
Recovering from a heart attack is a process that involves the healing of the heart muscle, and it takes time. Typically, the heart muscle healing may take several weeks following a heart attack. During this period, scar tissue forms in the damaged area, which helps in repairing the affected part of the heart. However, it’s important to note that the scar tissue is not as flexible as the original heart muscle, which can lead to some long-term effects on the heart’s pumping function.
To ensure a successful recovery and minimize the impact of a heart attack, several aspects of long-term treatment need to be considered. These include making significant lifestyle changes, adhering to prescribed medication, and participating in cardiac rehabilitation programs.
Lifestyle Changes
Your lifestyle plays a crucial role in your overall heart health. After a heart attack, it’s important to adopt a heart-healthy lifestyle to improve your chances of a full recovery and reduce the risk of future heart issues. Here are some lifestyle changes you may need to consider:
- Eating a balanced diet that includes plenty of fruits, vegetables, whole grains, and lean proteins.
- Managing your weight through portion control and regular physical activity.
- Avoiding smoking and limiting alcohol consumption.
- Engaging in regular exercise as recommended by your healthcare provider.
- Managing stress through techniques like meditation, deep breathing exercises, or engaging in hobbies.
Medication
Following a heart attack, your doctor may prescribe medication to manage the underlying risk factors and prevent future complications. It’s crucial to take your medications as prescribed, even if you start feeling better. Common medications prescribed after a heart attack include:
- Aspirin or other blood-thinning medications to reduce the risk of blood clots.
- Beta-blockers to lower blood pressure and reduce strain on the heart.
- ACE inhibitors or angiotensin receptor blockers (ARBs) to manage blood pressure and improve heart function.
- Statins to lower cholesterol levels and reduce the risk of plaque buildup in the arteries that could cause a heart attack when it stops the supply of oxygen to the heart.
Cardiac Rehabilitation
Cardiac rehabilitation programs are designed to help individuals recover and improve their heart health after a heart attack. These programs are tailored to each individual’s needs and may include:
- Exercise training to gradually build strength and endurance under medical supervision.
- Dietary guidance to promote heart-healthy eating habits.
- Education and counseling on managing risk factors and making necessary lifestyle changes.
- Psychological support to cope with the emotional and psychological impact of a heart attack.
Participating in a cardiac rehabilitation program can significantly contribute to your physical and emotional well-being, as well as enhance your overall quality of life.
By actively engaging in heart muscle healing through scar tissue formation, embracing long-term treatment strategies, making lifestyle changes, adhering to medication, and participating in cardiac rehabilitation programs, you can greatly improve your chances of a successful recovery and ensure a healthier future.
Differences between Heart Attacks and Cardiac Arrest
In our previous sections, we’ve explored the science behind heart attacks and the pathophysiology that triggers them. Now, let’s delve into the differences between heart attacks and cardiac arrest to deepen our understanding.
Heart Attack: A Circulation Problem
A heart attack, also known as myocardial infarction, occurs when there is a blockage in the flow of blood to the heart. This blockage, often caused by a buildup of plaque in the coronary arteries, restricts the circulation of oxygen-rich blood to the heart muscle. The lack of blood flow and oxygen can lead to damage or death of the heart tissue.
| Condition | Description |
| Heart Attack (Myocardial Infarction) | A circulation problem caused by a blockage in blood flow to the heart |
Cardiac Arrest: An Electrical Problem
Cardiac arrest, on the other hand, is an electrical problem that disrupts the heart’s normal rhythm, causing it to suddenly stop beating. The most common underlying rhythm during cardiac arrest is ventricular fibrillation, a chaotic and irregular heart rhythm that prevents the heart from effectively pumping blood to the body’s vital organs. Without immediate intervention, cardiac arrest can be fatal.
| Condition | Description |
| Cardiac Arrest | An electrical problem resulting in the sudden cessation of the heart’s pumping function |
It’s important to note that while a heart attack can lead to cardiac arrest, the two terms describe different aspects of cardiovascular emergencies. Each requires immediate medical attention but necessitates different treatments. Recognizing the signs and symptoms of both heart attacks and cardiac arrest is crucial for seeking appropriate help.
Unblocking Life: END
Months later, Amit’s life had taken a new turn. He felt more energetic, his health parameters improved, and he found joy in the little things he once overlooked.
As he played cricket with his children one evening, Amit realized the value of health. “It took a blocked artery to open my eyes,” he mused.
“Is your lifestyle nourishing your heart? Remember, it’s the small changes that unblock the path to a healthy heart.”
Conclusion
Understanding the science of heart attacks and their pathophysiology is crucial for your heart health. By gaining knowledge about heart attacks, you can recognize early symptoms, seek immediate medical help, and take appropriate steps for recovery. Prevention is key, and adopting a heart-healthy lifestyle plays a vital role in reducing your chances of experiencing a heart attack.
To maintain a healthy heart, it is important to manage risk factors such as high blood pressure, high cholesterol, and obesity. This can be achieved by avoiding smoking, maintaining a healthy weight, exercising regularly, and following a balanced diet. By managing stress and effectively treating other health conditions, you can further protect your heart.
If you have experienced a heart attack, recovery is possible. With proper treatment, lifestyle changes, and participation in cardiac rehabilitation programs, you can improve your heart health and lead a fulfilling life. It is essential to stay informed, work closely with your healthcare team, and prioritize your heart’s well-being.
Remember, prevention is always better than cure. By arming yourself with heart attack knowledge and taking proactive steps to prioritize your heart health, you can maintain a strong and resilient heart for years to come.
Key Takeaways:
- Understanding the science and pathophysiology of heart attacks is essential for recognizing the early signs.
- Atherosclerosis, the buildup of substances in the coronary arteries, plays a key role in causing heart attacks.
- Symptoms of a heart attack can vary but may include chest pain, pain spreading to the shoulder, arm, back, or jaw, cold sweat, fatigue, lightheadedness, and shortness of breath.
- Prompt treatment is crucial to prevent heart muscle damage.
- By recognizing the symptoms and understanding the underlying mechanisms, you can take proactive steps towards recovery and promote overall heart health.
FAQ Section Heart Attack Science and Pathophysiology
A: A heart attack, also known as a myocardial infarction, occurs when the blood flow to a part of the heart is blocked, usually by a blood clot. This blockage can cause damage to the affected part of the heart, leading to symptoms such as chest pain and shortness of breath.
A: The common symptoms of a heart attack include chest pain or discomfort, upper body pain or discomfort in the arms, back, neck, jaw, or stomach, shortness of breath, nausea, lightheadedness, and cold sweats.
A: Risk factors for a heart attack include high blood pressure, high cholesterol, smoking, obesity, diabetes, family history of heart disease, age, and a sedentary lifestyle.
A: A heart attack occurs when blood flow to a part of the heart is blocked, causing damage to the heart muscle. Without prompt treatment, the affected part of the heart muscle can die, leading to complications and potential long-term damage.
A: STEMI is a severe type of heart attack characterized by a complete blockage of a coronary artery, causing a significant portion of the heart muscle to be deprived of oxygen and nutrients. It requires immediate medical intervention to restore blood flow to the heart.
A: A heart attack is diagnosed through various methods such as electrocardiogram (ECG), blood tests to measure cardiac enzymes, coronary angiography, and imaging tests to assess the extent of heart damage.
A: Heart attacks are caused by a blockage in the flow of blood to the heart, usually due to the buildup of plaque in the coronary arteries, which can rupture and form a clot, leading to reduced blood flow or complete blockage to a part of the heart.
A: You can support a person who has had a heart attack by helping them adhere to their treatment plan, providing emotional support, encouraging a heart-healthy lifestyle, and assisting with activities as advised by their healthcare provider.
A: If you or someone else experiences symptoms that could indicate a heart attack, it is essential to call emergency services immediately. Time is of the essence in getting treatment for a heart attack.
A: Treatments for a heart attack may include medications to dissolve blood clots, angioplasty and stenting to open blocked arteries, coronary bypass surgery, and lifestyle changes to reduce the risk of another heart attack.
A: Coronary heart disease develops when the arteries that supply blood to the heart become narrowed or blocked by cholesterol and fatty deposits. This can lead to a heart attack if a blood clot forms and blocks the flow of blood to the heart.
A: During a heart attack, the blood supply to part of the heart muscle is cut off, causing damage to that portion of the heart. This can lead to complications such as abnormal heart rhythms, heart failure, or even sudden cardiac arrest.
A: Lifestyle changes such as quitting smoking, adopting a heart-healthy diet, engaging in regular physical activity, managing stress, controlling blood pressure and cholesterol levels, and taking prescribed medications can all help reduce the risk of heart attacks.
A: Assessing heart attack risk involves considering factors such as age, gender, family history, cholesterol levels, blood pressure, and lifestyle habits. An individual’s risk can be evaluated with the help of a healthcare provider and appropriate screening tests.
A: To lower your risk of having a heart attack, you can maintain a healthy diet, engage in regular physical activity, avoid smoking, manage stress, and monitor and manage any existing health conditions such as high blood pressure and diabetes.
A: A heart attack is typically diagnosed through a combination of medical history, physical examination, electrocardiogram (ECG), blood tests to detect cardiac enzymes, and imaging tests such as an echocardiogram or coronary angiography.
A: If you suspect someone is having a heart attack, call emergency services immediately, provide aspirin if available and the person is not allergic, and help the individual rest in a comfortable position while awaiting medical help.
A: A heart attack can cause damage to the heart by depriving a section of the heart muscle of oxygen and nutrients, resulting in the death of heart cells in that area. This can lead to reduced heart function and potential long-term impacts on overall heart health.
A: Treatment for NSTEMI may involve a combination of medications, such as antiplatelet drugs and anticoagulants, cardiac catheterization, and possibly angioplasty or stent placement to restore blood flow to the affected area of the heart.
A: To help prevent a future heart attack, it’s important to follow a heart-healthy lifestyle, attend regular medical check-ups, take prescribed medications as directed, and make necessary changes to your diet, exercise, and stress management routines as advised by your healthcare provider.
A: A widow-maker heart attack is a term used to describe a particularly severe type of heart attack that affects the left main coronary artery. This artery supplies a large portion of the heart muscle with blood, so a blockage in this artery can be life-threatening and is often referred to as a widow-maker due to its potential for sudden cardiac death.
A: Experiencing a heart attack while in the gym can be related to a pre-existing heart condition or risk factors such as high blood pressure, underlying heart disease, or atherosclerosis. Strenuous physical activity can put extra strain on the heart, and in some cases, trigger a heart attack, particularly in individuals with underlying cardiovascular issues.
A: The colder temperatures and changes in weather during winter can have an impact on the cardiovascular system. Cold weather can constrict blood vessels and increase blood pressure, which may make it harder for the heart to work efficiently. Additionally, the combination of cold weather, reduced physical activity, and higher calorie intake during the holiday season can contribute to a higher risk of heart attacks during winter.
A: No, not all heart attacks result in death. Quick medical intervention can significantly increase the chances of survival and minimize damage to the heart muscle.
