Are you aware of the impact that muscle tremors can have on the accuracy of electrocardiography (ECG) results? When your skeletal muscles shake, it can distort the ECG, leading to artifacts in the recordings. These artifacts can mimic various cardiac abnormalities, such as atrial fibrillation or flutter, and ventricular tachycardia.
Factors like tremors without an evident cause, Parkinson’s disease, anxiety, hyperthyroidism, certain medications, and shivering can contribute to these motion-induced errors in ECG recordings. To ensure accurate interpretations and avoid unnecessary interventions, it’s crucial to minimize these tremor-related errors.
Today, we’ll delve deeper into the impact of muscle tremors on ECG accuracy and discuss methods to reduce these artifacts effectively.
Key Takeaways:
- Muscle tremors can distort ECG recordings and mimic cardiac abnormalities.
- Factors such as tremors without an evident cause and certain medical conditions can contribute to these errors.
- Minimizing tremor-induced errors is essential for accurate ECG interpretations.
- Techniques like moving averaging and smoothing filters can help reduce tremor-related artifacts while preserving wave shape integrity.
- Continuous education of ECG technicians is vital in improving accuracy and minimizing the impact of muscle tremors.
Common Electrocardiographic Artifacts
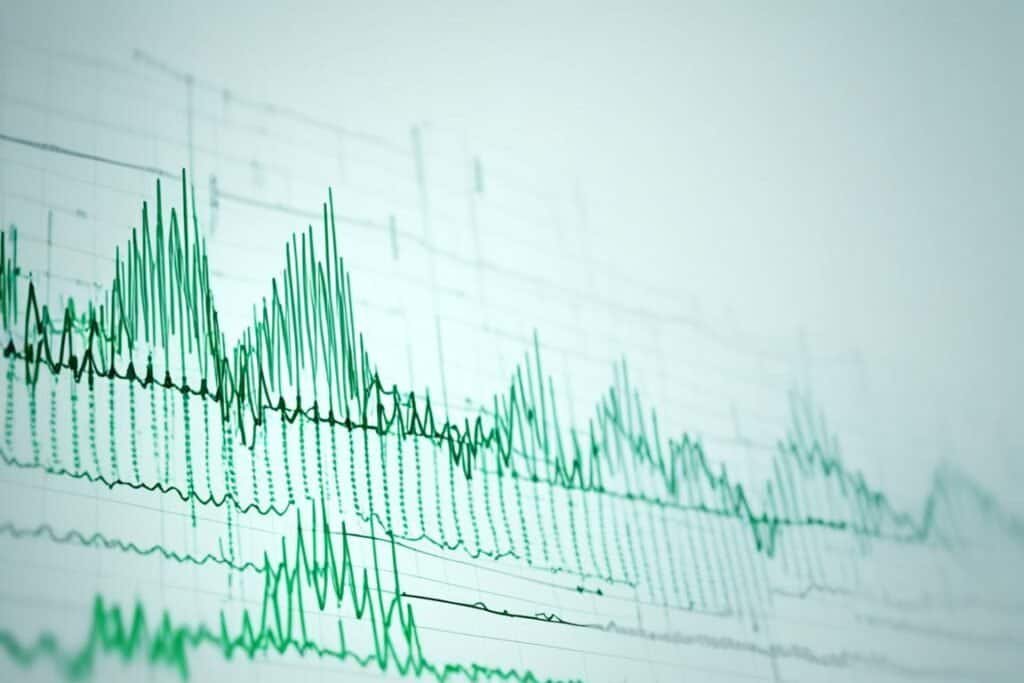
Electrocardiographic artifacts can arise from various sources, including motion and tremors. When the body experiences rhythmic movements, such as tremors, it can distort the baseline and waves of the ECG. These artifacts can resemble abnormal cardiac rhythms, causing interference in the interpretation of the ECG results. Some common causes of motion artifacts are:
- Tremors without an evident cause
- Parkinson’s disease
- Cerebellar or intention tremor
- Certain medications
These artifacts can pose a challenge in accurately diagnosing and interpreting ECG recordings. Additionally, other factors that contribute to electrocardiographic artifacts include electrode misplacement or incorrect interchange, electrical interference from devices in the room, and poor operation of the ECG device due to the lack of filters for alternating current systems.
To ensure accurate ECG interpretations, it is crucial for technicians who record ECGs to be continuously educated on identifying and minimizing these artifacts. This enables them to provide more reliable results and avoid unnecessary tests or interventions.
Effect of Tremors in Parkinson’s Disease
Parkinson’s disease and parkinsonian syndromes can have a significant impact on ECG recordings due to continuous muscle twitching, known as tremors. These tremors can be mistaken for atrial flutter, leading to misinterpretation of the ECG results. It is important to properly place the electrodes on the upper part of the arms and legs to eliminate the artifact of pseudo-atrial flutter caused by the tremors.
Tremors in Parkinson’s disease can also result in wide QRS complexes on the ECG, resembling ventricular tachycardia. This can further complicate the interpretation of the ECG recordings. Therefore, a careful analysis of the ECG and correlation with the patient’s clinical history are essential to differentiate between tremor artifacts and actual arrhythmias.
To accurately identify and differentiate tremor artifacts from true arrhythmias, healthcare professionals need to consider the patient’s medical history, symptoms, and other diagnostic tests alongside the ECG recordings. Additionally, appropriate electrode placement and thorough knowledge of the characteristic ECG patterns associated with Parkinson’s disease tremors are crucial for accurate interpretation.
By understanding the effects of tremors in Parkinson’s disease on ECG recordings and implementing appropriate strategies for interpretation, healthcare providers can minimize errors and ensure accurate diagnosis and treatment for patients with this complex condition.
Differentiating Tremors from Ventricular Tachycardia
Some ECG recordings may resemble ventricular tachycardia, but it is important to differentiate between actual arrhythmias and artifacts caused by tremors. These tremor-induced artifacts can mimic the characteristics of ventricular tachycardia, leading to potential misinterpretation and unnecessary interventions.
To distinguish between tremor artifacts and ventricular tachycardia, certain signs can be identified:
- Sinus Sign: Look for the presence of sinus rhythm with normal waves in one of the frontal leads. This indicates that the underlying rhythm is not ventricular tachycardia, but rather a tremor-related artifact.
- Spike Sign: Pay attention to small regular or irregular peaks between wide QRS complexes. These spikes are indicative of a tremor artifact rather than ventricular tachycardia.
- Notch Sign: Watch for overlapping notches in the artifact, coinciding with the duration of the cycle in which the sinus rhythm was recorded. This pattern confirms the presence of tremor-related artifacts.
By recognizing these signs, healthcare professionals can differentiate between tremors and ventricular tachycardia, ensuring accurate diagnoses and appropriate treatment plans.

| Sign | Description |
|---|---|
| Sinus Sign | Presence of sinus rhythm with normal waves in one of the frontal leads |
| Spike Sign | Small regular or irregular peaks between wide QRS complexes |
| Notch Sign | Overlapping notches in the artifact, coinciding with the duration of the cycle in which the sinus rhythm was recorded |
Mistaken Placement of Electrodes
Errors in the placement of electrodes during ECG recordings can lead to mistaken interpretations and mimic various rhythm or conduction abnormalities. One common error is the mistaken left arm-right arm reversal (LA/RA), which can result in negative P, QRS, and T waves in lead I, simulating a condition known as dextrocardia. However, correct placement of electrodes in the arms and legs can help differentiate between LA/RA reversal and actual dextrocardia based on the normal progression of QRS complexes.
There are several indicators that can suggest mistaken electrode placement. Unusual P-QRS patterns, negative P waves in leads aVL and I, positive P waves in lead III and aVR, as well as inverted or unchanged wave shapes, are all signs that electrode placement may be incorrect. Detecting these errors is crucial to ensure accurate ECG interpretations and prevent misdiagnosis.
To minimize mistaken electrode placement, computerized algorithms have been developed. These algorithms use artificial neural networks or correlation techniques between original and rebuilt leads to detect recurrent placement errors. By identifying and rectifying these errors, the accuracy of ECG recordings can be significantly improved.
Filtering and Suppression of Tremors in ECG Recordings
Various methods have been developed to filter and suppress tremors in ECG recordings. These techniques play a crucial role in minimizing tremor-induced artifacts and improving the accuracy of the recorded ECG waveform. Two commonly used methods for tremor suppression are moving averaging and Savitzky-Golay smoothing filter.
Moving Averaging
Moving averaging involves the use of a comb filter with a linear phase characteristic. This technique effectively suppresses both tremors and power-line interference simultaneously. By applying moving averaging, the reduced peaks of QRS complexes and other high and steep ECG waves can be restored. This restoration process ensures the preservation of useful high-frequency components, vital for accurate interpretation and diagnosis.
Savitzky-Golay Smoothing Filter
In addition to moving averaging, a Savitzky-Golay smoothing filter can be applied to further suppress tremors outside the QRS complexes. This filter effectively removes unwanted noise and artifacts, providing a cleaner and more reliable ECG recording. By utilizing this method, clinicians and technicians can obtain a more accurate representation of the cardiac electrical activity, facilitating accurate diagnosis and treatment planning.
These filtering and suppression techniques have proven to be highly effective in reducing tremor-related artifacts while preserving the integrity of the ECG waveform. The implementation of these methods can significantly enhance the accuracy of ECG interpretations, ultimately improving patient care and outcomes.
Conclusion
Muscle tremors can significantly impact the accuracy of ECG recordings, leading to artifact errors that mimic various cardiac abnormalities. It is crucial to identify and minimize these tremor-related artifacts to ensure precise interpretations and avoid unnecessary tests or interventions. Employing techniques such as moving averaging, linearly-angular restoration, and Savitzky-Golay smoothing filtering can effectively reduce tremor-induced errors while maintaining the integrity of the ECG waveform.
Continuous education of technicians involved in recording ECGs is essential for achieving higher accuracy and minimizing the impact of muscle tremors on ECG interpretations. By staying updated on the latest techniques and advances in minimizing artifact errors, technicians can make more informed decisions and provide reliable ECG results.
Ultimately, by prioritizing ECG accuracy and implementing strategies to minimize artifact errors caused by muscle tremors, healthcare professionals can ensure the reliability and validity of ECG interpretations. This, in turn, allows for better diagnosis, treatment, and management of cardiac conditions, leading to improved patient outcomes.

