
Introduction
If you or a loved one has been diagnosed with nephrotic syndrome, you may be wondering why cholesterol levels soar like a kite in the sky for patients with nephrotic syndrome? 🤔🪁 This blog is specially designed to unravel the mystery behind increased cholesterol levels in nephrotic syndrome, a chronic kidney disease.
In this friendly and motivating guide, we’ll explore the primary cause of elevated cholesterol in nephrotic syndrome – hyperlipidemia. This condition is characterized by high levels of lipids (fats) in the blood, leading to increased synthesis of very low-density lipoproteins (VLDL) in the liver. These VLDL particles, rich in cholesterol and triglycerides, contribute to the elevated cholesterol levels observed in patients.
We’ll also delve into how disruptions in lipoprotein metabolism, including reduced activity of key enzymes like lipoprotein lipase (LPL) and lecithin cholesterol acyl transferase (LCAT), further contribute to this dysregulation of lipid levels.
Join us in this enlightening journey to understand the intricacies of cholesterol management in nephrotic syndrome. It’s a straightforward read, yet packed with essential insights for anyone concerned about maintaining a healthy balance in their body. Let’s embark on this path of awareness and proactive health management together! ❤️🔬
A Brother’s Vow
Part – 1
In the bustling metropolis of Hyderabad, where the ancient and the modern blend seamlessly, Ashwin, a 38-year-old financial analyst, lived his life in the fast lane. His days were a whirlwind of numbers, meetings, and deadlines, leaving little room for anything else. At home, his world revolved around his younger sister, Jyoti, a vibrant 28-year-old who had recently been diagnosed with nephrotic syndrome, a condition Ashwin was struggling to understand amidst his hectic schedule.
Ashwin, known for his sharp analytical skills and emotional intelligence at work, found himself at a loss when it came to addressing Jyoti’s health condition. He had always believed in the power of hard work and determination to solve any problem, but this was a challenge that couldn’t be fixed with sheer willpower. Jyoti’s diagnosis revealed a deranged lipid profile with high cholesterol, a common but daunting aspect of nephrotic syndrome.
Pathology of Nephrotic Syndrome
Nephrotic syndrome is a collection of symptoms caused by kidney damage, often resulting from glomerular diseases such as glomerulosclerosis, membranous nephropathy, or minimal change disease. These kidney diseases can lead to abnormalities in the filtration process, resulting in proteinuria, reduced blood albumin levels, and elevated blood lipids, including cholesterol.
Signs of Hypercholesterolemia in Nephrotic Syndrome
Nephrotic syndrome leads to hypercholesterolemia. The lipid profile in these individuals is characterized by increased levels of low-density lipoproteins (LDL), very low-density lipoproteins (VLDL), and intermediate-density lipoproteins (IDL). Conversely, high-density lipoprotein (HDL) levels either remain normal or decrease. Additionally, hypertriglyceridemia, which refers to elevated triglyceride levels, is also observed in patients with nephrotic syndrome.
This dyslipidemia is a result of the underlying mechanisms of nephrotic syndrome and can have implications for the individual’s overall health. Understanding these lipid abnormalities is crucial in managing the condition and preventing associated complications.
LDL
Low-density lipoproteins (LDL) are commonly referred to as “bad” cholesterol due to their role in depositing cholesterol in the arteries. Elevated LDL cholesterol in patients of nephrotic syndrome can contribute to the development of atherosclerosis, increasing the risk of cardiovascular complications.
VLDL
Very low-density lipoproteins (VLDL) are responsible for transporting triglycerides from the liver to peripheral tissues. In nephrotic syndrome, increased VLDL levels contribute to the elevation of triglycerides and further exacerbate the dyslipidemia seen in these patients.
HDL
High-density lipoprotein (HDL), often referred to as “good” cholesterol, is responsible for removing excess cholesterol from the bloodstream and transporting it to the liver for disposal. In nephrotic syndrome, HDL levels may remain normal or decrease, impairing the body’s ability to eliminate excess cholesterol efficiently.
Hypertriglyceridemia
Nephrotic syndrome often presents with hypertriglyceridemia, marked by increased triglyceride levels. Increased production of VLDL by the liver and reduced breakdown of triglycerides contribute to the development of hypertriglyceridemia in these patients.
The table below summarizes the lipid abnormalities observed in nephrotic syndrome:
| Dyslipidemia Marker | Elevated/Decreased | Implications |
| LDL | Elevated | Risk of atherosclerosis and cardiovascular complications |
| VLDL | Elevated | Increased triglyceride levels and exacerbation of dyslipidemia |
| HDL | Normal/Decreased | Reduced cholesterol clearance and impaired lipid metabolism |
| Triglycerides | Elevated | Hypertriglyceridemia and increased cardiovascular risk |
The lipid abnormalities observed in nephrotic syndrome are reversible with appropriate management of the underlying condition. Treating nephrotic syndrome effectively can restore lipid levels to a more favorable range and reduce the risk of cardiovascular complications.
Mechanisms of LDL and Cholesterol Increase in Nephrotic Syndrome
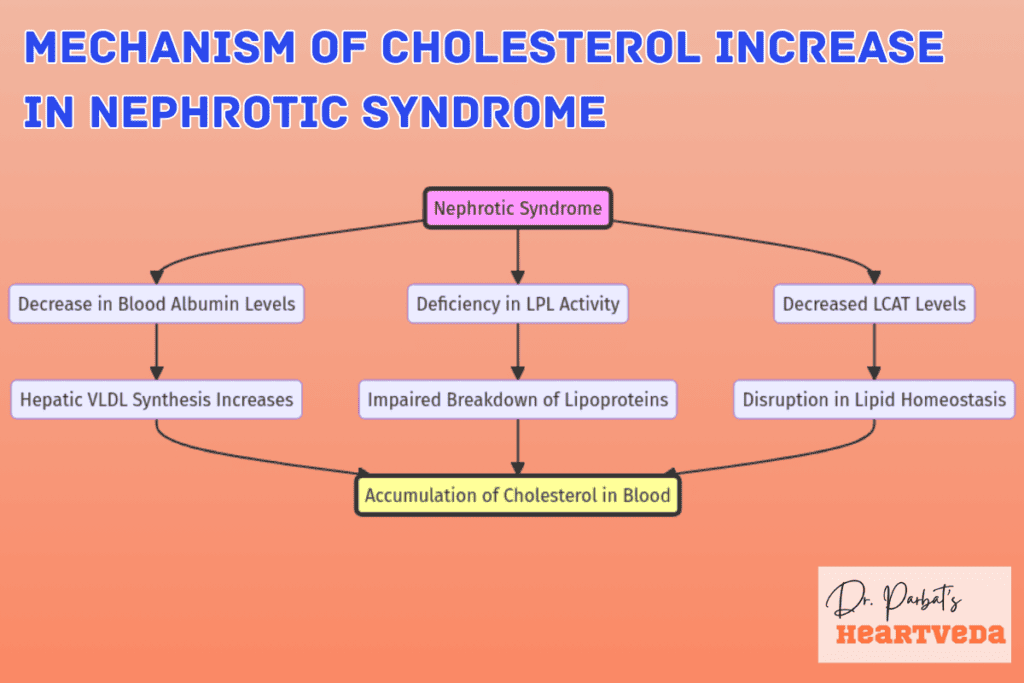
A deficiency in LPL activity impedes the breakdown of lipoproteins, including VLDL, leading to their accumulation in the bloodstream:
- Hepatic VLDL synthesis: The liver responds to the decrease in blood albumin levels by increasing the synthesis of very low-density lipoproteins (VLDL). This leads to elevated hepatic VLDL synthesis and contributes to the accumulation of cholesterol in the blood.
- Lipoprotein lipase (LPL) activity: Reduced activity of lipoprotein lipase, which is responsible for the degradation of VLDL, further exacerbates the accumulation of lipoproteins. This impaired breakdown of lipoproteins leads to increased cholesterol levels.
- Lecithin cholesterol acyl transferase (LCAT) levels: Decreased levels of lecithin cholesterol acyl transferase, an enzyme involved in cholesterol metabolism, disrupt lipid homeostasis. This disruption contributes to the dysregulation of cholesterol and further elevates cholesterol levels in nephrotic syndrome patients.
These mechanisms collectively contribute to the dyslipidemia observed in patients with nephrotic syndrome. The dysregulated cholesterol metabolism and impaired lipid homeostasis play significant roles in the elevation of cholesterol in these individuals.

- Total Cholesterol (TC), Triglycerides (TG), and Low-Density Lipoprotein (LDL): These are types of fats in the blood. The red bars represent the levels in patients with nephrotic syndrome, and they are higher than the levels in healthy controls (blue bars). High levels of these fats are generally considered unhealthy.
- High-Density Lipoprotein (HDL): This is often referred to as “good cholesterol”. In the patients (red bar), the levels are lower compared to the healthy controls (blue bar). Higher levels of HDL are usually better for health.
A Brother’s Vow
Part – 2
The realization that Jyoti’s condition required a comprehensive approach beyond medication was Ashwin’s wake-up call. His mental frame, which had always prioritized professional success over personal well-being, began to shift. The thought of his sister battling this condition alone, while he was consumed by work, brought him to his darkest moment.
Driven by a newfound determination, Ashwin began to educate himself about nephrotic syndrome. He learned that managing the condition involved a delicate balance of medications, lifestyle changes, and regular monitoring of Jyoti’s health. This knowledge transformed Ashwin, guiding him to support Jyoti in ways he hadn’t considered before.
Together, they embarked on a journey of recovery and wellness. Ashwin adjusted his work schedule to accompany Jyoti to her doctor’s appointments, where they met Dr. Reddy, a nephrologist who became their trusted advisor. Under Dr. Reddy’s guidance, they tackled Jyoti’s high cholesterol through a tailored diet plan rich in fruits, vegetables, and whole grains, and low in saturated fats. Exercise became a bonding activity for them, with evening walks and yoga sessions becoming a new routine.
Role of Lipoprotein Lipase (LPL) in Cholesterol Increase
In patients with nephrotic syndrome, the breakdown of triglyceride-rich lipoproteins, including VLDL, is impaired due to a deficiency of lipoprotein lipase (LPL). LPL plays a crucial role in the metabolism of lipoproteins, catalyzing their hydrolysis and subsequent clearance from the circulation. However, in individuals with nephrotic syndrome, urinary loss of apo C II and heparan sulfates, which are necessary for LPL activity, leads to reduced LPL levels and activity.
This deficiency in LPL activity hampers the breakdown of lipoproteins, including VLDL, resulting in their accumulation in the bloodstream. As a consequence, cholesterol levels in these patients become elevated, contributing to the hyperlipidemia observed in nephrotic syndrome.
“LPL deficiency caused by the urinary loss of apo C II and heparan sulfates disrupts the normal breakdown of lipoproteins, leading to increased cholesterol levels in the blood of individuals with nephrotic syndrome.”
The role of LPL deficiency in the pathogenesis of hyperlipidemia in nephrotic syndrome underscores the importance of understanding the mechanisms underlying lipid metabolism in kidney disease. By further elucidating the specific factors contributing to LPL deficiency and exploring potential therapeutic targets, researchers aim to develop interventions that can mitigate the dyslipidemia associated with nephrotic syndrome.
Abnormalities in Lipoprotein Metabolism in Nephrotic Syndrome
| Lipoprotein | Metabolic Abnormality |
| Very Low-Density Lipoproteins (VLDL) | Impaired breakdown due to LPL deficiency |
| Low-Density Lipoproteins (LDL) | Elevated levels |
| High-Density Lipoproteins (HDL) | Reduced synthesis and levels |
The presented table highlights the abnormalities observed in lipoprotein metabolism in nephrotic syndrome. While VLDL breakdown is impaired due to LPL deficiency, LDL levels are elevated, and HDL synthesis is reduced. These imbalances further contribute to the dyslipidemia observed in this condition.
The Role of Lecithin Cholesterol Acyl Transferase (LCAT) in Cholesterol Increase
In nephrotic syndrome, there is a reduction in Lecithin Cholesterol Acyl Transferase (LCAT) activity, leading to decreased high-density lipoprotein (HDL) synthesis. LCAT is an enzyme involved in the esterification of free cholesterol, which facilitates the transfer of cholesterol from peripheral tissues to HDL particles for transport.
LCAT deficiency disrupts the normal process of cholesterol metabolism, resulting in reduced HDL levels in the blood. HDL plays a crucial role in removing excess cholesterol from the body, and its reduction contributes to the elevation of cholesterol levels in individuals with nephrotic syndrome.
“LCAT deficiency in nephrotic syndrome impairs the esterification of cholesterol, leading to decreased HDL synthesis and compromised cholesterol transport.”
The decrease in HDL levels seen in nephrotic syndrome can adversely affect lipid balance and elevate the risk of cardiovascular complications. HDL helps remove excess cholesterol from tissues, inhibits inflammation, and promotes vasodilation, all of which are vital for maintaining cardiovascular health.
By understanding the role of LCAT deficiency in nephrotic syndrome, researchers and clinicians can focus on developing targeted therapies to restore normal LCAT activity and improve HDL synthesis. These approaches hold the potential to address the underlying dyslipidemia and reduce the risk of cardiovascular events in individuals with nephrotic syndrome.
Urinary Loss of HDL and Apo A1
The excessive proteinuria associated with nephrotic syndrome can lead to the urinary loss of HDL and its major protein component, apo A1. This loss further disturbs lipid metabolism and may contribute to the elevation of cholesterol levels in the blood.
Impact of Urinary Loss on HDL and Apo A1
Proteinuria, the presence of excess proteins in the urine, is a hallmark of nephrotic syndrome. One of the proteins that can be lost through proteinuria is high-density lipoprotein (HDL), commonly known as “good cholesterol.” HDL plays a vital role in transporting cholesterol from peripheral tissues back to the liver for metabolism and excretion.
Apo A1, the major protein component of HDL, is directly involved in the reverse cholesterol transport process. It helps in removing excess cholesterol from arteries and facilitates its transport to the liver for elimination. However, in nephrotic syndrome, the urinary loss of HDL and apo A1 disrupts this essential lipid transport mechanism, impacting overall cholesterol metabolism.
Consequences of Urinary Loss on Lipid Metabolism
The urinary loss of HDL and apo A1 in nephrotic syndrome contributes to dyslipidemia, characterized by elevated levels of cholesterol, triglycerides, and other lipids in the blood. This abnormal lipid profile significantly increases the risk of cardiovascular disease, such as heart attacks and strokes.
In addition, the decreased levels of HDL, a protective factor against atherosclerosis, reduce the efficiency of cholesterol removal from artery walls. This, combined with the elevated levels of LDL (low-density lipoprotein), also known as “bad cholesterol,” further promotes the development of plaques and increases the risk of cardiovascular events.
The urinary loss of HDL and apo A1 in nephrotic syndrome not only contributes to dyslipidemia but also potentiates the progression of kidney damage. The impaired lipid metabolism can lead to oxidative stress, inflammation, and endothelial dysfunction, resulting in glomerular fibrosis and worsening of nephrotic syndrome.
| Effects of HDL and Apo A1 Urinary Loss | Consequences |
| Impaired reverse cholesterol transport | Increased cholesterol deposition in peripheral tissues |
| Reduced efficiency in cholesterol removal | Promotion of atherosclerosis and cardiovascular disease |
| Inflammation and oxidative stress | Progression of kidney damage and glomerular fibrosis |
Therefore, Managing the urinary loss of HDL and apo A1 in nephrotic syndrome is essential to reduce its impact on lipid metabolism and alleviate associated complications.
Atherogenic Effects of Lipid Abnormalities in Nephrotic Syndrome
Although the atherogenic effects of lipid abnormalities in nephrotic syndrome are not well-established, they may contribute to complications such as platelet aggregation, thrombus formation, and glomerular fibrosis.
Abnormal lipid levels can promote the formation of blood clots and reduce the immune response, potentially leading to cardiovascular complications and worsening kidney damage.
Treatment of Lipid Abnormalities in Nephrotic Syndrome
Treatment of hypercholesterolemia in nephrotic syndrome involves a comprehensive approach that addresses the underlying condition and related factors such as high blood pressure and elevated blood cholesterol levels. Treatment options include lifestyle modifications, medication, and regular monitoring of lipid levels.
Lifestyle Modifications
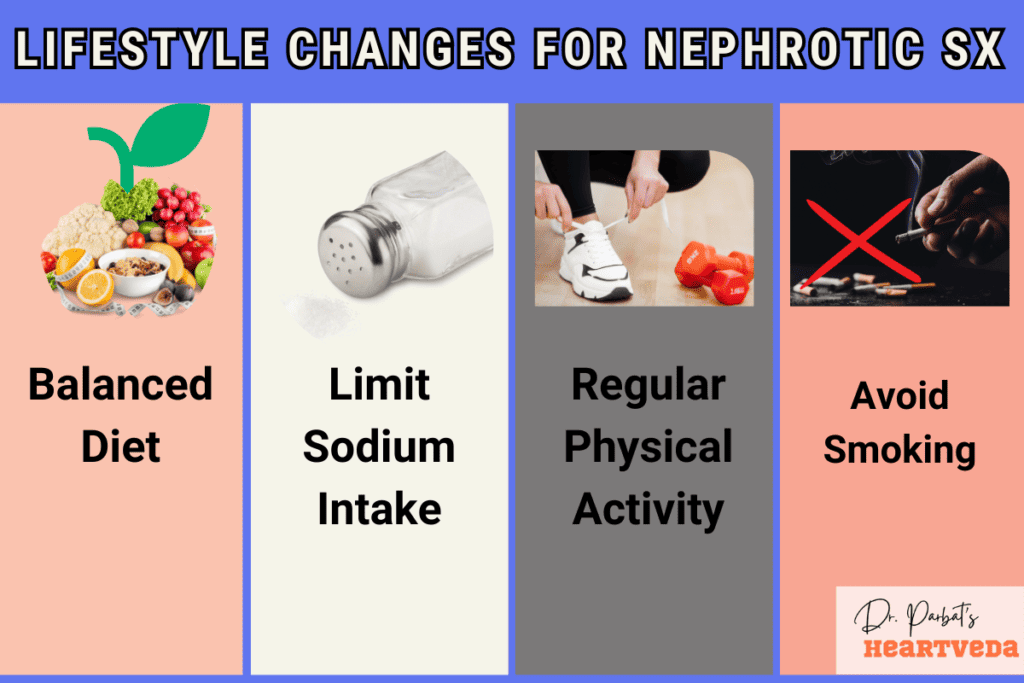
Adopting a healthy lifestyle is an essential aspect of managing hyperlipidemia in nephrotic syndrome. Here are some recommended lifestyle modifications:
- Follow a balanced diet: Consume a diet low in saturated fats, trans fats, and cholesterol. Increase the intake of fruits, vegetables, whole grains, and lean proteins.
- Limit sodium intake: Reduce the consumption of salty foods, as excessive sodium can lead to fluid retention and high blood pressure.
- Engage in regular physical activity: Incorporate exercise into your daily routine to promote cardiovascular health and maintain a healthy weight.
- Avoid smoking: Smoking can worsen the effects of hyperlipidemia, increase the risk of cardiovascular complications, and negatively impact kidney function.
- Limit alcohol consumption: Excessive alcohol intake can raise blood pressure and cholesterol levels, leading to further complications.
Medication
In some cases, lifestyle modifications alone may not be sufficient to control hyperlipidemia in nephrotic syndrome. Your healthcare provider may prescribe medications to help manage your lipid levels. Commonly prescribed medications include:
- Statin drugs: Statins are medications that lower cholesterol levels by inhibiting an enzyme involved in cholesterol production. They are effective in reducing LDL cholesterol levels and may also have additional cardiovascular benefits.
- Fibrates: Fibrates work by decreasing triglyceride levels and increasing HDL cholesterol levels. They are often prescribed to address the dyslipidemia associated with nephrotic syndrome.
It is important to follow your healthcare provider’s instructions when taking these medications and to attend regular follow-up appointments to monitor your progress.
Regular Monitoring
To effectively manage hyperlipidemia in nephrotic syndrome, regular monitoring of lipid levels is crucial. Your healthcare provider may recommend periodic blood tests to assess your cholesterol profile and determine the effectiveness of the treatment plan. Based on the results, adjustments to medications or lifestyle modifications may be made to optimize your lipid control.
Remember, managing hyperlipidemia in nephrotic syndrome requires a multi-faceted approach that combines lifestyle modifications, medication, and regular monitoring. By working closely with your healthcare provider and following the recommended treatment plan, you can effectively control your lipid levels and reduce the risk of complications.
A Brother’s Vow
END
This shared journey brought Ashwin and Jyoti closer than ever before. Ashwin’s perspective on life and health underwent a profound transformation. He realized that success wasn’t just about professional achievements but also about being there for the ones you love, helping them fight their battles.
Their story is a testament to the power of knowledge, empathy, and action in the face of chronic illness. It highlights the message that managing conditions like nephrotic syndrome requires a holistic approach, encompassing not just medical treatment but also lifestyle adjustments and the support of loved ones. The question it leaves us with is, are we ready to prioritize health and family over the relentless pursuit of success?
Complications of Hyperlipidemia in Nephrotic Syndrome
Hyperlipidemia in nephrotic syndrome can lead to a range of complications that significantly impact the health of patients. The elevated levels of cholesterol and altered lipid metabolism associated with nephrotic syndrome contribute to the development of:
- Blood Clots: Increased cholesterol levels can promote the formation of blood clots, which can lead to serious cardiovascular events such as deep vein thrombosis or stroke. The risk of blood clots is particularly significant in individuals with nephrotic syndrome, as the abnormal lipid profile can disrupt normal blood circulation.
- Infections: Nephrotic syndrome weakens the immune system, making individuals more susceptible to infections. The altered lipid metabolism in these patients further compromises immune function, increasing the risk of infections, including respiratory infections and urinary tract infections.
- High Blood Pressure: Hyperlipidemia in nephrotic syndrome can contribute to the development of high blood pressure, also known as hypertension. Elevated cholesterol levels and the resulting damage to blood vessels can lead to increased resistance to blood flow, contributing to hypertension and its associated health complications.
It is vital to manage hyperlipidemia effectively in patients with nephrotic syndrome to minimize the risk of these complications. By controlling cholesterol levels through lifestyle modifications, appropriate medications, and addressing underlying factors such as high blood pressure, healthcare providers can help mitigate the adverse effects of hyperlipidemia in nephrotic syndrome.
| Complications | Description |
| Blood Clots | Promote the formation of blood clots, increasing the risk of cardiovascular events. |
| Infections | Compromised immune function and increased susceptibility to infections. |
| High Blood Pressure | Contribution to the development of hypertension, increasing risk of related complications. |
Implications for Research and Future Treatment Approaches
Ongoing research is continuously working towards a better understanding of the underlying mechanisms behind elevated cholesterol levels in nephrotic syndrome. By uncovering these mechanisms, researchers hope to develop more targeted treatments that can effectively manage hyperlipidemia in these patients. The aim is to improve cholesterol metabolism and address the specific abnormalities observed in lipoprotein synthesis and degradation.
The potential treatment approaches being explored include:
- Dietary interventions: Research is investigating the impact of specific dietary modifications on cholesterol metabolism in nephrotic syndrome. This includes exploring the effects of modifying macronutrient ratios, restricting certain dietary components, and optimizing nutrient intake.
- Pharmacological interventions: Scientists are exploring the potential of novel medications or repurposing existing drugs to target the unique lipid abnormalities observed in nephrotic syndrome. These treatments may focus on improving lipid metabolism, regulating hepatic VLDL synthesis, enhancing lipoprotein degradation, or enhancing HDL synthesis.
- Genetic studies: Researchers are conducting genetic studies to identify genetic variants and mutations that may contribute to the dyslipidemia seen in nephrotic syndrome. Understanding the genetic basis of the condition can help in developing personalized treatments and therapies.
By identifying effective treatment strategies, future research endeavors aim to alleviate the burden of hyperlipidemia in nephrotic syndrome and improve the overall quality of life for affected individuals.
“Understanding the complex interplay between cholesterol metabolism and nephrotic syndrome is crucial for unlocking new treatment options and improving patient outcomes.”
Treatment Approaches in Development
Ongoing research is providing promising insights into potential therapies for managing hyperlipidemia in nephrotic syndrome. Here are a few notable approaches being explored:
| Treatment Approach | Key Focus |
| Targeted Therapy | Developing medications that specifically address the underlying abnormalities in lipid metabolism, such as enhancing LPL activity or restoring LCAT levels. |
| Gene Therapy | Investigating the potential of gene therapy to correct genetic mutations associated with dyslipidemia in nephrotic syndrome and restore normal lipid metabolism. |
| Immunomodulation | Exploring the use of immunomodulatory agents to regulate the immune response and reduce proteinuria, thus indirectly impacting lipid metabolism. |
Although these treatments hold promise, additional research is required to confirm their efficacy and safety prior to their clinical implementation.
Conclusion
In conclusion, nephrotic syndrome is characterized by elevated cholesterol levels, which can be attributed to various abnormalities in cholesterol metabolism. Increased hepatic VLDL synthesis, reduced LPL activity, and decreased LCAT levels contribute to the dyslipidemia observed in these patients. Understanding the underlying mechanisms of hyperlipidemia in nephrotic syndrome is crucial for the development of effective treatment strategies and the management of associated complications.
Further research is needed to explore novel therapeutic approaches aimed at improving cholesterol metabolism and addressing the specific abnormalities in lipoprotein synthesis and degradation observed in patients with nephrotic syndrome. By advancing our understanding of these mechanisms, we can pave the way for more targeted and personalized treatments, ultimately improving outcomes for individuals with nephrotic syndrome and associated hyperlipidemia.
As healthcare professionals, it is important to recognize the impact of dyslipidemia in nephrotic syndrome and to prioritize the management of cholesterol levels in these patients. By implementing lifestyle modifications, such as dietary changes and regular physical activity, and considering medications like statins or fibrates, we can effectively control hyperlipidemia and reduce the risk of complications such as blood clots, infections, and high blood pressure.
In summary, the management of hyperlipidemia in nephrotic syndrome requires a comprehensive approach that addresses the underlying causes while also focusing on individual patient needs. With ongoing research and advances in technology, there is hope for improved treatment options and better outcomes for individuals with nephrotic syndrome and associated hyperlipidemia.
Key Takeaways:
- Nephrotic syndrome is a chronic kidney disease that leads to symptoms such as edema, decreased blood protein levels, and elevated cholesterol.
- Elevated cholesterol in nephrotic syndrome is primarily caused by hyperlipidemia, which results from increased synthesis of VLDL in the liver.
- Abnormalities in lipoprotein metabolism, including reduced LPL activity and decreased LCAT levels, also contribute to the elevated cholesterol levels observed in nephrotic syndrome.
Q: What is the relationship between hyperlipidemia and the nephrotic syndrome?
A: The nephrotic syndrome often leads to hyperlipidemia, a condition characterized by high levels of lipids such as cholesterol and triglycerides in the blood. This is due to increased synthesis and decreased catabolism of lipoproteins.
Q: What are the mechanisms underlying dyslipidaemia in the nephrotic syndrome?
A: The dyslipidaemia in the nephrotic syndrome is primarily attributed to increased hepatic synthesis of lipoproteins and a reduction in the clearance of very low-density lipoprotein (VLDL) particles. Additionally, there is a decrease in the activity of lipoprotein lipase and hepatic lipase, leading to elevated triglycerides and cholesterol levels.
Q: How does the treatment of nephrotic syndrome impact hyperlipidemia?
A: Treatment of nephrotic syndrome often involves the use of corticosteroids, which can induce changes in lipid metabolism and reduce hyperlipidemia. In addition, other therapeutic interventions such as statins may be utilized to lower cholesterol levels and mitigate the effects of hyperlipidemia in nephrotic patients.
Q: What are the consequences of untreated hyperlipidemia in patients with the nephrotic syndrome?
A: Untreated hyperlipidemia in patients with the nephrotic syndrome can increase the risk of cardiovascular complications such as atherosclerosis, coronary artery disease, and stroke. It can also contribute to the progression of renal dysfunction and exacerbate the existing proteinuria.
Q: How is the dyslipidaemia in nephrotic syndrome managed in pediatric patients?
A: In pediatric patients with nephrotic syndrome, the management of dyslipidaemia often involves dietary modifications aimed at reducing saturated fat and cholesterol intake. Additionally, medications such as statins may be prescribed to address elevated lipid levels in children with nephrotic syndrome.
Q: What are the effects of simvastatin and cholestyramine in the treatment of hyperlipidemia in nephrotic patients?
A: Simvastatin, a statin medication, is used to inhibit cholesterol synthesis and reduce LDL levels in nephrotic patients. Cholestyramine, a bile acid sequestrant, can also be employed to lower cholesterol by binding to bile acids in the intestine, ultimately decreasing cholesterol absorption.
Q: How does dyslipidaemia in the nephrotic syndrome impact lipid metabolism?
A: Dyslipidemia in the nephrotic syndrome disrupts lipid metabolism by increasing the production of VLDL and LDL and decreasing the catabolism of these lipoproteins. This leads to elevated levels of triglycerides and cholesterol in the blood, contributing to the development of hyperlipidemia.
Q: What are the treatment options for hyperlipidemia in patients with the nephrotic syndrome?
A: Treatment options for hyperlipidemia in patients with the nephrotic syndrome include lifestyle modifications such as diet and exercise, as well as pharmacological interventions such as statins, fibrates, and bile acid sequestrants. These measures are aimed at reducing cholesterol and triglyceride levels, thereby mitigating the effects of hyperlipidemia.
Q: What are the complications associated with hyperlipidaemia in the context of nephrotic syndrome?
A: Complications associated with hyperlipidemia in the context of nephrotic syndrome include an increased risk of developing atherosclerosis, cardiovascular disease, and renal impairment. These complications necessitate the management of hyperlipidemia to mitigate its adverse effects on overall health and well-being.
Q: How does chronic renal disease contribute to dyslipidaemia in patients with the nephrotic syndrome?
A: Chronic renal disease in patients with the nephrotic syndrome can contribute to dyslipidaemia by altering lipid metabolism and impairing the renal clearance of lipoproteins. This results in elevated levels of cholesterol and triglycerides, further exacerbating the existing hyperlipidaemia in nephrotic patients.
Q: What is the relationship between nephrotic syndrome and hyperlipidemia?
A: Nephrotic syndrome often leads to hyperlipidemia, characterized by elevated levels of LDL and cholesterol due to altered lipid metabolism in the body.
Q: What are the mechanisms of hyperlipidemia in nephrotic syndrome?
A: The mechanisms include increased synthesis of triglycerides and cholesterol, decreased clearance of lipoproteins, and altered expression of lipid-regulating proteins.
Q: How is hyperlipidemia in the nephrotic syndrome detrimental to health?
A: Elevated levels of cholesterol and triglycerides increase the risk of atherosclerosis, cardiovascular disease, and other complications associated with nephrotic syndrome.
Q: What are the consequences of high cholesterol in patients with nephrotic syndrome?
A: Patients with nephrotic syndrome are at a higher risk of developing heart disease and other cardiovascular complications due to elevated levels of serum cholesterol.
Q: What is the treatment for hyperlipidemia in nephrotic syndrome?
A: Treatment may involve dietary modifications, lipid-lowering medications such as statins, and management of the underlying kidney disease to improve lipid metabolism.
Q: How is hyperlipidemia in the nephrotic syndrome managed in children?
A: Children with nephrotic syndrome and hyperlipidemia may require a specialized approach in treatment, including careful monitoring and age-appropriate interventions to control lipid levels.
Q: Is experimental nephrotic syndrome in nephrotic rats used to study lipid metabolism?
A: Yes, experimental nephrotic syndrome in nephrotic rats is often utilized to study the pathophysiology of hyperlipidemia in nephrotic syndrome and evaluate potential treatments.
Q: What is nephrotic range proteinuria and its association with hyperlipidemia?
A: Nephrotic range proteinuria refers to significant protein loss in urine, which contributes to the development of hyperlipidemia through complex mechanisms in the body.
Q: How does hypertriglyceridemia manifest in patients with nephrotic syndrome?
A: Hypertriglyceridemia is commonly observed in patients with nephrotic syndrome, further exacerbating the lipid profile and increasing the risk of cardiovascular complications.
Q: Are there specific treatments targeting lipid metabolism in nephrotic syndrome to prevent cardiovascular complications?
A: Research is ongoing to identify specific treatments that target lipid metabolism and reduce the risk of cardiovascular complications in patients with nephrotic syndrome and associated hyperlipidemia.
