When it comes to heart attacks, recognizing the early signs is crucial for timely intervention and potentially saving lives. Understanding how heart attack pain starts and being aware of the symptoms can help you take the necessary steps to seek immediate medical attention. In this section, we will explore the early warning signs of a heart attack, with a specific focus on chest pain.
Heart Attack Symptoms in Men and Women
When it comes to heart attacks, recognizing the warning signs is crucial. While both men and women may experience chest pain or discomfort, there are other symptoms that can manifest differently between the genders. It’s important to be aware of these differences to ensure timely intervention and appropriate medical care.
In Men:
- Chest pain or discomfort that may feel like pressure, squeezing, fullness, or pain
- Pain or discomfort in other areas of the upper body, such as the arms, back, neck, jaw, or stomach
- Shortness of breath, with or without chest discomfort
- Breaking out in a cold sweat
- Nausea or lightheadedness
In Women:
- Chest pain or discomfort, similar to men
- Shortness of breath
- Nausea or vomiting
- Back or jaw pain
It’s important to note that women may experience symptoms that are not commonly associated with heart attacks, such as back or jaw pain. Recognizing these signs can help save lives by prompting immediate medical attention.
Remember, the key signs of a heart attack are not limited to chest pain alone. If you experience any of the symptoms mentioned, it’s crucial to call for emergency medical assistance immediately. Every minute counts when it comes to saving lives.
| Symptom | Men | Women |
|---|---|---|
| Chest pain or discomfort | ✓ | ✓ |
| Pain or discomfort in other areas of the upper body | ✓ | ✓ |
| Shortness of breath | ✓ | ✓ |
| Breaking out in a cold sweat | ✓ | – |
| Nausea or lightheadedness | ✓ | – |
| Back or jaw pain | – | ✓ |
| Nausea or vomiting | – | ✓ |
The Importance of Calling Emergency Medical Servcies
Recognizing the early signs of a heart attack is crucial for timely intervention and potentially saving lives. If you experience any symptoms of a heart attack, it is important to call medical emergency services immediately, even if you are unsure. Fast action can significantly increase the chances of survival and reduce the risk of long-term complications.
When you call medical emergency services(EMS) teams are dispatched to your location. These highly trained professionals are equipped to provide immediate medical treatment and transport you to the nearest hospital. By calling medical emergency services, you ensure that an experienced EMS team can start treatment right away and arrange for rapid transport to the emergency room for further evaluation and care.
It is important to note that heart attack symptoms can vary from person to person. While chest pain is the most common symptom, it can also manifest differently in some individuals. The pain may be located in the chest, but it can also radiate to other areas of the upper body, such as the arms, back, neck, jaw, and stomach. Additionally, some people may experience other warning signs like shortness of breath, breaking out in a cold sweat, nausea, or lightheadedness.
Remember, minutes matter when it comes to a heart attack. By calling medical emergency services, you are taking a vital step towards receiving appropriate medical care as quickly as possible.
| Heart Attack Warning Signs | Heart Attack Pain Location | What Does a Heart Attack Feel Like |
|---|---|---|
| The pain may be located in the chest and can also radiate to other areas of the upper body, such as the arms, back, neck, jaw, and stomach. | Heart attack pain can vary from person to person. It can feel like pressure, squeezing, fullness, or pain in the chest. Other symptoms may include shortness of breath, breaking out in a cold sweat, nausea, or lightheadedness. |
Understanding Heart Attack Causes
Heart attacks are often caused by various factors, including coronary artery disease (CAD), plaque buildup, and coronary artery spasms. It is essential to understand these causes to help identify potential risk factors and take necessary preventive measures.
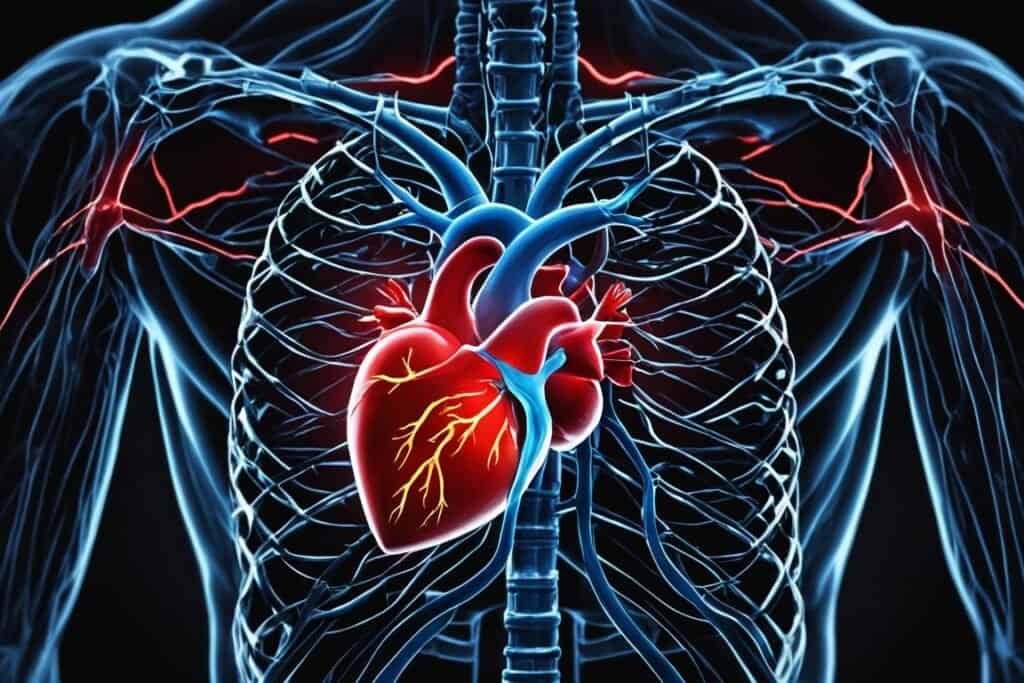
Coronary Artery Disease (CAD)
CAD is the primary cause of most heart attacks. It occurs when there is a buildup of plaques consisting of fat, cholesterol, and other substances in the coronary arteries. Over time, these plaques can narrow the arteries, restricting blood flow to the heart. Reduced blood flow can lead to angina (chest pain) and, in severe cases, can trigger a heart attack.
Plaque Buildup
Plaque buildup is a gradual process that occurs over time. It starts with the accumulation of cholesterol and other substances in the arterial walls. As the plaques grow, they harden and narrow the arteries, reducing blood flow. If a plaque ruptures, it can cause blood clots to form, further blocking the arteries and increasing the risk of a heart attack.
Coronary Artery Spasm
In some cases, a coronary artery may experience a severe spasm or sudden contraction, leading to a heart attack. This spasm causes the artery to narrow or close completely, blocking the blood supply to the heart muscle. Coronary artery spasms can occur in individuals with or without significant plaque buildup.
Less Common Causes
While CAD, plaque buildup, and coronary artery spasms are the primary causes of heart attacks, certain infections and spontaneous coronary artery dissection (SCAD) can also lead to heart attacks. Infections such as endocarditis (infection of the heart valves) or myocarditis (inflammation of the heart muscle) can weaken the heart muscle and increase the risk of a heart attack. SCAD is a rare condition where the layers of the coronary artery wall separate, potentially blocking the blood flow to the heart.
To better understand the causes of a heart attack, it is crucial to consult with a healthcare professional who can assess your individual risk factors and provide personalized guidance for prevention.
Identifying Heart Attack Risk Factors
Understanding the risk factors associated with heart attacks is crucial for assessing your own risk and taking preventive measures. Several factors contribute to an increased risk of experiencing a heart attack. By recognizing these risk factors, you can make necessary lifestyle changes to protect your heart health.
Age: As you grow older, the risk of heart attacks tends to increase. Men aged 45 and above and women aged 55 and above are more susceptible to heart attacks.
Tobacco Use: Smoking and exposure to secondhand smoke are significant risk factors for heart attacks. Quitting smoking is the most effective way to reduce this risk and improve overall cardiovascular health. Seek support from healthcare professionals and explore smoking cessation programs for assistance.
High Blood Pressure: Having high blood pressure, or hypertension, puts strain on your heart and increases the risk of a heart attack. Regular monitoring of blood pressure levels and adhering to prescribed treatments can help manage this risk factor.
High Cholesterol: Elevated levels of LDL cholesterol, also known as “bad” cholesterol, can lead to the buildup of plaque in the arteries and increase the risk of a heart attack. Adopting a heart-healthy diet and following a prescribed medication regimen can help control cholesterol levels.
Obesity: Carrying excess weight, especially around the waist, increases the likelihood of developing various cardiovascular conditions, including heart attacks. Maintaining a healthy weight through regular physical activity and a balanced diet is essential to mitigate this risk factor.
Diabetes: People with diabetes are at a higher risk of heart attacks due to the adverse effects of high blood sugar on blood vessels. Proper management of blood sugar levels through medication, diet, and exercise is crucial in reducing the risk of heart attacks and other complications.
Family History: If you have close relatives who have experienced heart attacks, you may have a higher predisposition to develop the condition. Genetic factors can play a role, but lifestyle modifications can still help manage this risk factor.
By understanding these heart attack risk factors and taking proactive steps, such as making lifestyle changes and managing associated health conditions, you can significantly reduce your risk of experiencing a heart attack. It is important to prioritize your heart health and work in close collaboration with healthcare professionals to ensure a healthy future.
Potential Heart Attack Complications
Heart attack complications can occur as a result of damage to the heart muscle. These complications can have serious consequences and require prompt medical attention and treatment to prevent or manage them effectively.
Irregular Heart Rhythms (Arrhythmias): One potential complication of a heart attack is the development of irregular or atypical heart rhythms. This can disrupt the normal electrical signals that control the heart’s rhythm, leading to heart palpitations, fluttering sensations, or a racing heartbeat. Arrhythmias can be managed with medication or other interventions.
Cardiogenic Shock: Another possible complication is cardiogenic shock, which occurs when the heart fails to pump enough blood to meet the body’s needs. This can lead to organ damage and even death if left untreated. Prompt medical intervention, such as medications, oxygen therapy, or mechanical support devices, is crucial in managing cardiogenic shock.
Heart Failure: Heart failure is the inability of the heart to adequately pump blood to meet the body’s needs. It can occur immediately after a heart attack or develop gradually over time. Symptoms may include fatigue, shortness of breath, swelling in the legs, and fluid retention. Treatment for heart failure may involve medications, lifestyle changes, and possible surgical interventions.
Inflammation of the Sac Surrounding the Heart (Pericarditis): Pericarditis involves the inflammation of the sac surrounding the heart. This can cause chest pain, which may worsen with deep breaths or when lying down. The treatment for pericarditis may involve medications to reduce inflammation and manage pain, as well as addressing the underlying cause.
Cardiac Arrest: In some cases, a heart attack can lead to cardiac arrest, which is the sudden stopping of the heart. This is a life-threatening emergency that requires immediate intervention through CPR (cardiopulmonary resuscitation) and potentially defibrillation to restore normal heart rhythm.
It is crucial to understand and recognize these potential complications of a heart attack. Seeking immediate medical attention during a heart attack and receiving appropriate treatment can significantly reduce the risk of these complications and improve outcomes.
Summary of Heart Attack Complications
| Complication | Description |
|---|---|
| Irregular Heart Rhythms | Disruption of normal heart rhythm, leading to palpitations and racing heartbeat |
| Cardiogenic Shock | Failure of the heart to pump enough blood, resulting in organ damage |
| Heart Failure | Inability of the heart to adequately pump blood, causing symptoms such as fatigue and shortness of breath |
| Inflammation of the Sac Surrounding the Heart (Pericarditis) | Inflammation of the sac surrounding the heart, leading to chest pain |
| Cardiac Arrest | Sudden stopping of the heart, requiring immediate life-saving interventions |
Steps for Recovery After a Heart Attack
After experiencing a heart attack, it is important to take proactive steps towards a successful recovery. Your healthcare team will guide you through the process and provide specific recommendations tailored to your condition. Here are some essential steps to consider:
- Discuss Physical Activity with Your Healthcare Team: Physical activity is an integral part of the recovery process. However, it is essential to consult your healthcare team before starting any exercise routine. They will provide guidance on the appropriate level of activity and any limitations you may need to consider initially.
- Adopt a Healthier Diet: Making dietary changes is crucial for improving heart health. Incorporate more fruits, vegetables, whole grains, lean proteins, and healthy fats into your daily meals. Limit the intake of saturated fats, trans fats, cholesterol, sodium, and added sugars.
- Increase Physical Activity: Gradually increase your physical activity level under the guidance of your healthcare team. Engage in activities such as walking, swimming, cycling, or low-impact aerobic exercises. Regular exercise improves cardiovascular health, reduces the risk of future heart problems, and helps maintain a healthy weight.
- Quit Smoking: If you are a smoker, quitting smoking is crucial for your heart health. Smoking significantly increases the risk of heart attacks and other cardiovascular conditions. Seek support from healthcare professionals, join cessation programs, and consider nicotine replacement therapies if needed.
- Manage Stress: Stress can have a negative impact on your heart health. Adopt stress management techniques such as deep breathing exercises, meditation, yoga, or engaging in activities you enjoy. Prioritize self-care and take time for relaxation and rejuvenation.
- Consider Cardiac Rehabilitation: Cardiac rehabilitation programs are specialized programs that encompass physical activity, education, and counseling to support heart attack recovery. These programs can be instrumental in improving your physical fitness, managing risk factors, and reducing the likelihood of future health problems.
To support your recovery, it is essential to follow your healthcare team’s recommendations diligently. By making these necessary lifestyle changes and participating in cardiac rehabilitation programs, you can enhance your heart health, improve overall well-being, and reduce the risk of future heart complications.
Conclusion
Preventing heart attacks and maintaining heart health require timely intervention and a proactive approach. By recognizing the early signs of a heart attack and understanding the risk factors, you can take the necessary steps to protect yourself and your loved ones.
When you experience the warning signs of a heart attack, such as chest discomfort or pain, shortness of breath, or other related symptoms, don’t hesitate to call medical emergency services. Seek immediate medical attention to increase the chances of survival and minimize long-term complications.
Additionally, adopting a heart-healthy lifestyle is crucial for heart attack prevention. Take care of your body by managing risk factors like smoking, high blood pressure, high cholesterol levels, obesity, diabetes, and a family history of heart attacks. Maintain a balanced diet, engage in regular physical activity, quit smoking, and manage stress effectively.
Lastly, after a heart attack, prioritize your recovery by following a comprehensive plan recommended by your healthcare team. Embrace lifestyle changes, attend cardiac rehabilitation programs, and continue to take proactive steps to ensure a healthier life moving forward. Remember, your heart health is in your hands.
Key Takeaways:
- Recognizing the early signs of a heart attack is essential for prompt medical intervention.
- Chest pain is a common symptom of a heart attack, often described as pressure, squeezing, fullness, or pain.
- Other areas of the upper body, such as the arms, back, neck, jaw, and stomach, may also experience pain or discomfort.
- Shortness of breath, breaking out in a cold sweat, nausea, or lightheadedness are additional warning signs that require attention.
- If you experience any of these symptoms, it is important to call medical emergency services immediately and seek medical help.
