Welcome to our article on the fascinating connection between non-alcoholic fatty liver disease (NAFLD) and cholesterol metabolism. NAFLD is a prevalent liver disorder that often occurs in individuals with obesity and metabolic syndrome. It encompasses various liver injuries, from simple fatty liver to more severe conditions like fibrosis and cirrhosis.
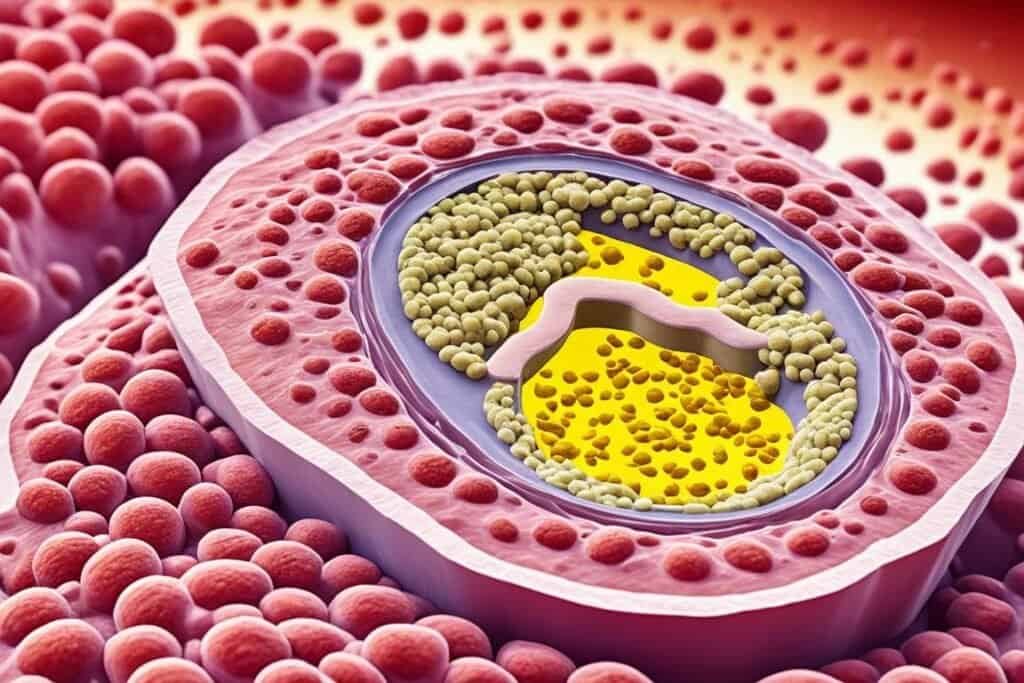
While the accumulation of fat in the liver is a hallmark feature of NAFLD, recent research suggests that alterations in cholesterol metabolism also play a role in its development and progression. Cholesterol, a vital component of cellular membranes and a precursor for various molecules, is tightly regulated to maintain balance in the body.
In this article, we will explore the intricate relationship between NAFLD and cholesterol metabolism, highlighting their impact on each other. By understanding these connections, we can gain insights into potential therapeutic interventions and preventive measures for NAFLD.
But first, let’s delve into the fascinating interplay between non-alcoholic fatty liver disease and cholesterol metabolism.
Key Takeaways:
- Non-alcoholic fatty liver disease (NAFLD) is commonly associated with obesity and metabolic syndrome.
- Cholesterol metabolism plays a crucial role in NAFLD development and progression.
- Imbalances in cholesterol input and output pathways contribute to NAFLD.
- Elevated cholesterol levels and dyslipidemia are observed in patients with NAFLD.
- Understanding the relationship between NAFLD and cholesterol metabolism is crucial for effective interventions.
Cholesterol Homeostasis and NAFLD
Cholesterol homeostasis plays a crucial role in the development and progression of non-alcoholic fatty liver disease (NAFLD). Understanding the intricate balance between cholesterol input and output pathways is key to comprehending the pathophysiology of NAFLD and its association with cardiovascular disease.
In the body, cholesterol is acquired through two main processes: endogenous synthesis in the liver and absorption from the diet. It is then transported in the bloodstream by lipoproteins.
- Endogenous synthesis: Cholesterol is synthesized in the liver from precursor molecules. This process is tightly regulated and influenced by various factors including dietary intake, hormones, and genetic factors.
- Dietary absorption: Intestinal cholesterol absorption is a major contributor to cholesterol homeostasis. The Niemann-Pick C1 Like 1 (NPC1L1) transporter mediates the absorption of cholesterol from the diet. It is estimated that around 60% of cholesterol in the body comes from dietary sources.
Once cholesterol is acquired, it undergoes several steps in maintaining homeostasis:
- Cholesterol packaging and transport: Cholesterol is esterified and packaged into chylomicrons for transport to the liver.
- Intrahepatic metabolism: In the liver, cholesterol is synthesized, stored, and eventually secreted into bile or converted into bile acids.
- Peripheral tissue transport: Cholesterol is transported from peripheral tissues back to the liver by high-density lipoproteins (HDL).
Imbalances in these processes can disrupt cholesterol homeostasis and contribute to the development of NAFLD. For instance, increased cholesterol synthesis in the liver or excessive dietary cholesterol intake may lead to cholesterol overload in the liver, triggering the formation of fatty liver and subsequent progression to more severe forms of NAFLD.
By understanding and targeting the mechanisms involved in cholesterol homeostasis, researchers aim to develop new strategies for the prevention and treatment of NAFLD. Further investigations into the complex interplay between cholesterol metabolism and NAFLD are needed to unveil potential therapeutic avenues.
Cholesterol and the Pathophysiology of NAFLD
Observational studies have linked Non-Alcoholic Fatty Liver Disease (NAFLD) with an increased risk of cardiovascular disease (CVD), suggesting a potential link between cholesterol metabolism and NAFLD. Patients with NAFLD often exhibit dyslipidemia characterized by elevated triglycerides and decreased high-density lipoprotein (HDL) cholesterol levels. While total low-density lipoprotein (LDL) cholesterol levels may not be increased, there is evidence of elevated levels of atherogenic LDL subpopulations in patients with NAFLD.
Animal models fed high-cholesterol diets have shown the development of both early NAFLD lesions and atherosclerosis. These findings indicate a possible association between cholesterol overload, NAFLD, and atherosclerosis.
Systemic Inflammation and the Progression of NAFLD
One of the key factors influencing the progression of Non-Alcoholic Fatty Liver Disease (NAFLD) is systemic inflammation. Research studies have demonstrated that systemic inflammation can worsen both atherosclerosis and NAFLD induced by cholesterol overload. In fact, in animal models, the introduction of additional systemic inflammation has been shown to lead to the development of advanced NAFLD lesions and atherosclerosis. This suggests that systemic inflammation has a significant impact on both the liver and the arteries in the context of NAFLD and atherosclerosis.

These findings highlight the complex relationship between inflammation, NAFLD, and its associated complications. Inflammation not only contributes to the development and progression of NAFLD but can also further exacerbate atherosclerosis, increasing the risk of cardiovascular disease. The expression of toll-like receptors (TLRs), which are inflammatory cellular receptors, was found to increase in the aorta, indicating the involvement of systemic inflammation in the progression of NAFLD and its impact on multiple organs.
Understanding the role of systemic inflammation in the pathogenesis of NAFLD is crucial for developing effective therapeutic strategies. By targeting systemic inflammation, healthcare professionals can potentially slow down the progression of NAFLD and reduce the risk of associated complications, such as atherosclerosis and cardiovascular disease.
Conclusion
Non-alcoholic fatty liver disease (NAFLD) has a significant impact on cholesterol metabolism. The imbalances in cholesterol input and output pathways can contribute to the development and progression of NAFLD. Emerging evidence suggests that increased cellular cholesterol is involved in the pathophysiology of NAFLD and its association with cardiovascular disease.
Additionally, systemic inflammation can exacerbate both NAFLD and atherosclerosis induced by cholesterol overload. It is crucial to understand the intricate relationship between NAFLD and cholesterol metabolism to develop effective therapeutic interventions for NAFLD and its associated complications. By targeting cholesterol homeostasis and reducing systemic inflammation, we may be able to prevent or slow down the progression of NAFLD and reduce the risk of cardiovascular complications.
Overall, the understanding of non-alcoholic fatty liver disease and its impact on cholesterol metabolism has opened up new avenues for research and treatment. By addressing the underlying factors contributing to NAFLD, such as cholesterol imbalances and inflammation, we can hope to improve the outcomes for individuals with this condition and reduce the burden of cardiovascular disease in the population.