Introduction
Have you ever pondered the connection between a heart attack and a stroke? 🤔💔 These two health scares, often striking without warning, are like unwelcome guests in the lives of busy Indian professionals. This blog aims to unravel the mystery behind their link, offering a beacon of understanding in a sea of medical jargon.
In simple terms, we’re setting sail to explore the relationship between heart attacks and strokes, two formidable foes of our health. While they may seem like distant relatives, their roots intertwine through shared risk factors such as high blood pressure, cholesterol, and lifestyle choices. 🌱➡️❤️🧠
With a friendly and motivating tone, we’ll guide you through the signs and symptoms of each, emphasizing the importance of early detection and prevention. Imagine your body as a complex network of roads; heart attacks and strokes are the traffic jams that block the flow, causing chaos in the system. By understanding how to maintain clear pathways, you can navigate towards a healthier future.
This blog is your compass, pointing towards actionable insights and preventive measures to keep both heart attacks and strokes at bay. Let’s embark on this journey together, armed with knowledge and the power to change our health destiny. 🚀🌟
The Unseen Connection
Part – 1
In the bustling heart of Bangalore, where the dawn breaks with the promise of endless possibilities and the night falls with the weight of unfinished tasks, lived Priya, a 38-year-old software developer. Her life was a tapestry of code, deadlines, and back-to-back meetings, a relentless pursuit of excellence that left little room for pause.
Priya’s family, a supportive husband and a teenage daughter, often echoed the silence of her absence, feeling her presence more in the whirlwind of her departure than in quiet moments shared. Priya, known for her sharp analytical skills and high emotional intelligence, adeptly managed her team’s dynamics and project challenges. Yet, she struggled to apply this wisdom to her own life, trapped in a mental frame that equated rest with regression.
Understanding Heart Attacks and Strokes
Heart attacks and strokes are life-threatening medical emergencies that can occur due to problems with blood flow. A heart attack, as mentioned before, happens when blood flow to a coronary artery is blocked, leading to damage to the heart muscle. A stroke, on the other hand, occurs when blood flow to the brain is interrupted, either due to a clot or the rupture of a blood vessel. Both conditions can be caused by factors such as a buildup of plaque in the arteries, which narrows the blood vessels and reduces blood flow. It is important to recognize the signs and symptoms of both conditions to ensure immediate medical treatment.
Heart attacks, also known as myocardial infarctions, occur when there is a blockage in the coronary arteries. The coronary arteries supply oxygen-rich blood to the heart muscle. When one or more of these arteries become blocked, it can lead to damage or death of the heart muscle. This can result in chest pain, shortness of breath, and other symptoms.
Strokes, also known as cerebrovascular accidents, occur when there is a disruption in blood flow to the brain. This can be caused by a clot that blocks a blood vessel or the rupture of a blood vessel, leading to bleeding in the brain. Strokes can cause a wide range of symptoms, including weakness or numbness on one side of the body, difficulty speaking, vision changes, and severe headaches.
Risk factors for heart attacks and strokes include high blood pressure, high cholesterol, smoking, obesity, diabetes, a sedentary lifestyle, and a family history of cardiovascular disease. It is important to manage these risk factors through lifestyle modifications such as regular exercise, a healthy diet, maintaining a healthy weight, quitting smoking, and controlling chronic conditions such as diabetes and high blood pressure.
Early recognition of the signs and symptoms of heart attacks and strokes is crucial for prompt medical treatment. Seeking immediate medical attention can help reduce the damage caused by these conditions and improve the chances of a successful recovery.
This table outlines the key symptoms to watch for in heart attacks and strokes, with the recommended immediate action to take if these symptoms appear.
Symptoms of a Heart Attack
A heart attack, also known as a myocardial infarction, is a medical emergency that occurs when there is a blockage or reduced blood flow to the coronary arteries, resulting in damage to the heart muscle. Recognizing the symptoms of a heart attack is crucial for prompt medical intervention, as it can help save lives.
Common symptoms of a heart attack include:
- Chest pain or discomfort: This is the most common symptom of a heart attack. It can feel like pressure, squeezing, or fullness in the chest.
- Upper body discomfort: Pain or discomfort may be felt in the arms, shoulders, neck, jaw, or back.
- Pain that radiates down the left arm: Many people experience pain or discomfort in the left arm, although it can also affect the right arm.
- Shortness of breath: Difficulty breathing or a feeling of being out of breath can occur during a heart attack.
- Cold sweat: Profuse sweating, often accompanied by clamminess, is a common symptom.
- Tiredness: Unusual fatigue or exhaustion can be a sign of a heart attack.
- Nausea: Feeling nauseous or vomiting can occur in some cases.
- Lightheadedness or dizziness: A feeling of lightheadedness or dizziness may be present during a heart attack.
It is important to note that not all heart attacks involve chest pain, and symptoms can vary among individuals. Women may experience different symptoms from men during a heart attack. Some of these symptoms include:
- Sudden weakness: Feeling weak or having difficulty moving.
- Shortness of breath: Difficulty breathing or feeling breathless.
- Body aches: Generalized pain or discomfort in the body.
- Sleep problems: Having trouble sleeping or feeling restless.
- Nausea and vomiting: Feeling sick to the stomach and vomiting.
- Indigestion: Discomfort or pain in the upper abdomen, similar to heartburn.
If you experience any of these symptoms, especially chest pain, shortness of breath, or upper body discomfort, it is essential to seek immediate medical attention. Acting quickly can help minimize damage to the heart and improve the chances of a successful recovery.
Symptoms of a Stroke
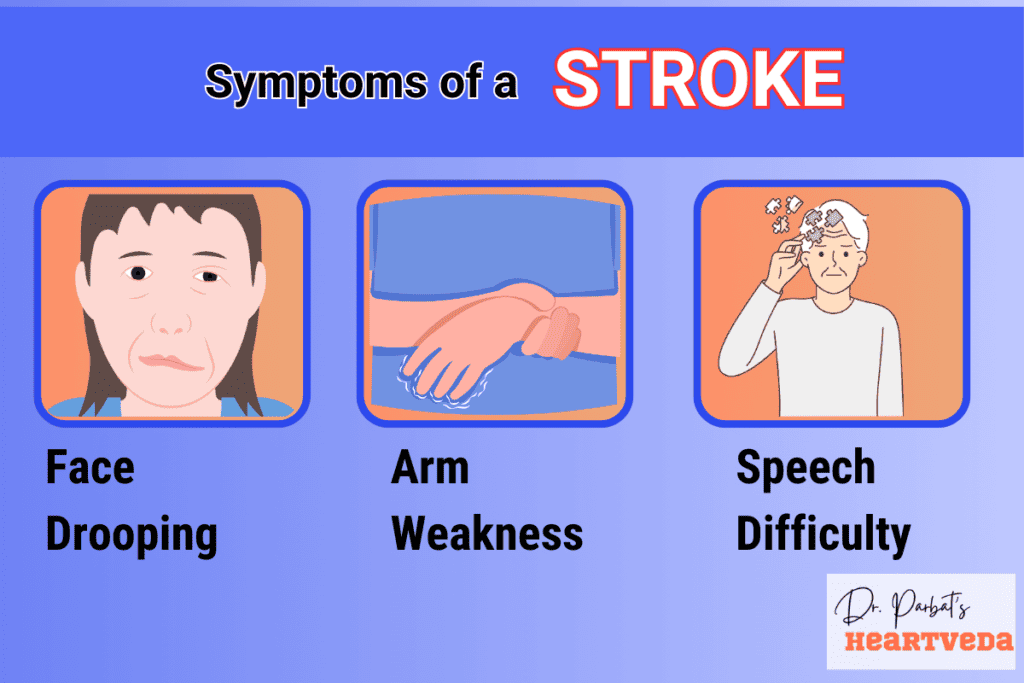
When it comes to recognizing a stroke, understanding the symptoms is crucial for prompt medical attention. The signs of a stroke can vary depending on the part of the brain affected and the severity of the damage. Here are the most common symptoms to watch out for:
- Sudden Numbness or Weakness: You may experience sudden numbness or weakness in the face, arm, or leg, typically on one side of the body.
- Confusion or Difficulty Speaking: You might find yourself struggling with speech or having difficulty understanding what others are saying.
- Sudden Difficulty Walking or Loss of Balance: A stroke can cause sudden difficulties with walking, balance, or coordination.
- Trouble Seeing: Vision problems can occur in one or both eyes, making it challenging to see clearly.
- Sudden Severe Headache: A stroke can often manifest as a sudden and severe headache, which is different from a regular headache.
It’s important to remember the acronym FAST (Face drooping, Arm weakness, Speech difficulty, Time to call emergency medical service) when identifying stroke symptoms. If you or someone around you experiences any of these symptoms, don’t hesitate to seek immediate medical help. Time is of the essence when it comes to stroke treatment, and early intervention can greatly improve the chances of a positive outcome.
Symptoms of Heart Attack vs Stroke
| Condition | Chest Discomfort | Discomfort in Other Upper Body Areas | Shortness of Breath | Other Signs | Face Drooping | Arm Weakness | Speech Difficulty | Emergency Action |
|---|---|---|---|---|---|---|---|---|
| Heart Attack | Feels like pressure or pain in the center of the chest, which might come and go. | May feel pain or discomfort in the arms, back, neck, jaw, or stomach. | Can happen with or without chest pain. | Might sweat a lot, feel sick to the stomach, or feel dizzy. | Not a sign of a heart attack. | Not a sign of a heart attack. | Not a sign of a heart attack. | Call emergency medical service for any heart attack symptoms. |
| Stroke | Not a usual sign. | Not a usual sign. | Not a usual sign, unless there is another health issue. | Not usual signs of a stroke. | The face may sag or feel numb, and smiling may be difficult. | One arm may be weak or drop down when trying to lift both. | Speech may be unclear or hard to understand; repeating a simple phrase may be hard. | Call emergency medical service right away if there are any signs of a stroke, even if they stop. |
The Unseen Connection
Part – 2
The consequence of her relentless pace came crashing down one evening when Priya experienced a heart attack. It was a moment that shattered her illusion of control, plunging her into a darkness she had never anticipated. This event marked her life’s darkest chapter, forcing her to confront the fragility of her existence.
The journey to recovery introduced Priya to Anand, a fellow patient who had suffered a stroke. Despite their different professions—Anand being a high-flying marketing executive—their stories were mirror images of each other, woven from threads of unyielding stress, inadequate rest, and neglected health. Their shared experiences forged a bond of understanding and mutual support.
Through her conversations with Anand, Priya realized that their health crises, though medically distinct, were rooted in similar lifestyles. This revelation was her turning point. Guided by healthcare professionals and buoyed by Anand’s companionship, Priya embarked on a path of profound transformation.
Risk Factors for Heart Attacks and Strokes
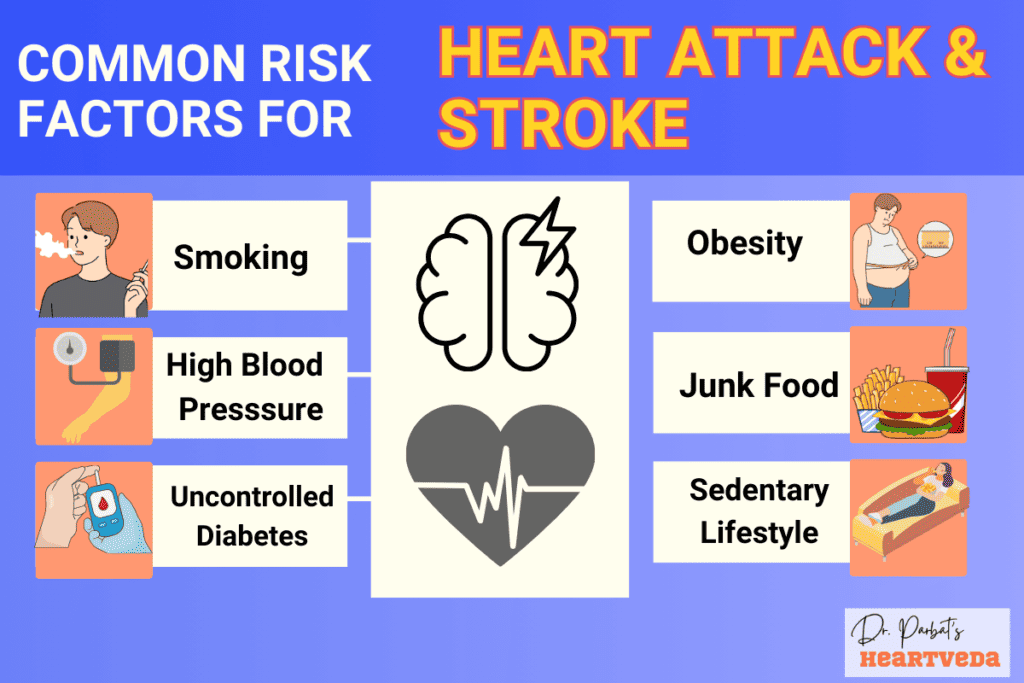
Certain risk factors increase the likelihood of experiencing a heart attack or stroke. It is important to be aware of these risk factors and make lifestyle modifications to reduce the chances of a heart attack or stroke.
High Blood Pressure
High blood pressure, also known as hypertension, is a significant risk factor for heart attacks and strokes. When blood pressure remains elevated over time, it puts strain on the arteries, causing damage and increasing the risk of cardiovascular diseases. Regular monitoring of blood pressure and following a healthcare provider’s advice can help manage this risk factor.
High Cholesterol
High levels of cholesterol and triglycerides in the blood can lead to the formation of plaque in the arteries, narrowing the blood vessels and reducing blood flow. This buildup of plaque increases the risk of heart attacks and strokes. Making dietary changes, exercising regularly, and, if necessary, taking medications as prescribed can help lower cholesterol levels and reduce the risk.
Smoking
Smoking is a major risk factor for heart attacks and strokes. The chemicals in tobacco smoke damage blood vessels, promote the build-up of plaque, and increase the risk of blood clots. Quitting smoking is the most effective way to reduce this risk factor. It is never too late to quit, and support is available through healthcare providers, helplines, and cessation programs.
Other Risk Factors
In addition to high blood pressure, high cholesterol, and smoking, other risk factors include obesity, diabetes, a poor diet, a lack of physical activity, drinking too much alcohol, and stress. Individuals with a family history of stroke or heart attack, advanced age, certain racial or ethnic backgrounds, and specific medical conditions are also at an increased risk. It is important to address these risk factors and adopt a heart-healthy lifestyle to reduce the chances of a heart attack or stroke.
Differences between a Heart Attack and a Stroke
While both heart attacks and strokes involve impaired blood flow, they affect different parts of the body and have distinct symptoms. A heart attack occurs when blood flow to the heart is blocked, leading to chest pain and other symptoms. A stroke, on the other hand, occurs when blood flow to the brain is interrupted, resulting in symptoms such as numbness, confusion, and difficulty speaking. It is crucial to recognize the differences between these conditions to seek appropriate medical treatment.
Summary of Key Differences
| Heart Attack | Stroke | |
| Causes | Chest pain, heart muscle damage | Interrupted blood flow to the brain |
| Body Part Affected | Heart | Brain |
| Common Symptoms | Chest pain, upper body discomfort, shortness of breath, cold sweat, tiredness, nausea, lightheadedness or dizziness | Numbness, confusion, difficulty speaking, difficulty walking, trouble seeing, severe headache |
| Treatment | Immediate medical attention, medication, procedures like angioplasty or stenting | Immediate medical attention, medication, rehabilitation therapy |
Distinguishing between a heart attack and a stroke is crucial as the appropriate treatment varies for each condition. When experiencing symptoms such as chest pain, it is important to consider the possibility of a heart attack, while symptoms such as sudden weakness or difficulty speaking may indicate a stroke. Seeking immediate medical attention can significantly improve the chances of a positive outcome.
The Effects of Paralysis on the Cardiovascular System
Paralysis, whether from trauma or disease, can have significant effects on the cardiovascular system. In particular, damage to the Autonomic Nervous System (ANS) can disrupt the normal functioning of the heart and blood vessels. Paralysis can increase the risk of complications such as obesity, insulin resistance, diabetes, dyslipidemia, hypertension, deconditioning, and inflammation. It is important for individuals with paralysis to be aware of these risks and take steps to manage them.
When paralysis affects the Autonomic Nervous System, it can lead to a condition called autonomic dysfunction. This dysfunction impairs the body’s ability to regulate its cardiovascular responses, such as heart rate, blood pressure, and blood vessel constriction. As a result, individuals with paralysis may experience abnormalities in these vital functions.
Risk of Obesity
Paralysis can increase the risk of obesity due to decreased physical activity and changes in metabolism. Individuals with paralysis often have decreased muscle mass and decreased ability to burn calories, leading to weight gain. Obesity, in turn, can put additional strain on the cardiovascular system and increase the risk of other cardiovascular conditions.
Risk of Insulin Resistance and Diabetes
Paralysis can also increase the risk of insulin resistance and diabetes. Insulin resistance refers to the decreased ability of the body’s cells to respond to insulin, a hormone that regulates blood sugar levels. As a result, individuals with paralysis may have difficulty controlling their blood sugar levels, leading to an increased risk of developing diabetes. Diabetes, in turn, can further increase the risk of cardiovascular complications.
Risk of Dyslipidemia
Damage to the Autonomic Nervous System can also lead to dyslipidemia, which refers to abnormal levels of cholesterol and triglycerides in the blood. Individuals with paralysis may have imbalances in their lipid profile, increasing the risk of cardiovascular disease. It is crucial for individuals with paralysis to monitor their cholesterol and triglyceride levels and take appropriate measures, such as adopting a healthy diet and lifestyle, to prevent further complications.
Risk of Hypertension
Hypertension, or high blood pressure, is a common cardiovascular condition that individuals with paralysis may be prone to. The Autonomic Nervous System plays a crucial role in regulating blood pressure, and damage to this system can cause abnormalities in blood pressure control. It is important for individuals with paralysis to monitor their blood pressure regularly and work with healthcare professionals to manage hypertension effectively.
Risk of Deconditioning and Inflammation
Due to decreased physical activity and muscle disuse, individuals with paralysis may experience deconditioning, which refers to the loss of muscular strength and cardiovascular fitness. Deconditioning can further exacerbate the cardiovascular risks associated with paralysis. Additionally, inflammation may occur as a result of the underlying damage or trauma that caused the paralysis, further impacting the cardiovascular system. It is important for individuals with paralysis to engage in appropriate physical therapy and rehabilitation programs to minimize deconditioning and manage inflammation.
| Risks | Complications |
| Obesity | Increased strain on the cardiovascular system |
| Insulin resistance and diabetes | Elevated blood sugar levels, increased risk of cardiovascular disease |
| Dyslipidemia | Abnormal cholesterol and triglyceride levels, increased risk of cardiovascular disease |
| Hypertension | High blood pressure, increased risk of cardiovascular complications |
| Deconditioning and inflammation | Loss of muscular strength, cardiovascular fitness, and increased risk of inflammation on the cardiovascular system |
It is essential for individuals with paralysis to work closely with healthcare professionals to manage these cardiovascular risks. Regular medical check-ups, lifestyle modifications, and adherence to prescribed medications or therapies can help minimize the complications associated with paralysis on the cardiovascular system.
The Unseen Connection
Part – 3
She learned to value her well-being, integrating exercise, mindful eating, and, crucially, periods of rest into her daily routine. These changes, initially daunting, gradually became sources of strength, illuminating her path to wellness with the light of hope and resilience.
Priya’s recovery was not just a return to health but a journey towards a balanced life, where success and well-being walked hand in hand. Her story, shared with colleagues and loved ones, became a beacon of awareness, highlighting the vital message that heart attack and stroke, though distinct, share a common ground in prevention through lifestyle modification.
Physical Assessments for Cardiac Risk
Various physical assessments can help determine the risk of cardiovascular disease. These assessments provide valuable insights into the individual’s heart health and overall cardiovascular risk. The three key physical assessments for assessing cardiac risk are pulse assessment, blood pressure measurement, and waist circumference measurement.
Pulse Assessment
Pulse assessment involves measuring the heart rate and strength of the pulse. The pulse provides vital information about the heart’s rhythmicity and efficiency of blood circulation. A healthy resting heart rate ranges between 60 and 100 beats per minute. An irregular or abnormal pulse may indicate underlying heart issues that require further evaluation.
Blood Pressure Measurement
Blood pressure measurement assesses the pressure in the blood vessels and indicates the force exerted by the circulating blood on the vessel walls. It is represented by two values: systolic pressure (the higher number) and diastolic pressure (the lower number). A normal blood pressure reading is around 120/80 mmHg. Elevated blood pressure increases the strain on the heart and blood vessels, increasing the risk of cardiovascular diseases such as heart attack and stroke.
Waist Circumference Measurement
Waist circumference measurement provides an indicator of obesity and increased cardiovascular risk. Excess abdominal fat, as indicated by an increased waist circumference, is associated with a higher risk of developing heart disease, diabetes, and other health conditions. In general, a waist circumference of more than 35 inches for women and 40 inches for men is considered a risk factor for cardiovascular disease.
Additionally, medical professionals may conduct other assessments such as EKG (electrocardiogram) and stress tests to evaluate cardiac function and identify any underlying abnormalities or conditions that may increase cardiac risk.
| Assessment | Measurement | Normal Range | Indication of Risk |
| Pulse Assessment | Heart rate and strength of pulse | 60-100 beats per minute | Irregular or abnormal pulse |
| Blood Pressure Measurement | Systolic and diastolic pressure | Around 120/80 mmHg | Elevated blood pressure |
| Waist Circumference Measurement | Measurement of waist circumference | Less than 35 inches for women and 40 inches for men | Increased waist circumference |
Stroke Awareness and Prevention
Despite being a leading cause of death and disability, stroke awareness is significantly lacking in India. Many people ignore the minor symptoms of stroke, delaying medical attention and increasing the risk of complications. It is crucial to understand the signs and symptoms of stroke and seek immediate medical help. Additionally, awareness of the multiple risk factors for stroke, such as hypertension, diabetes, and high cholesterol, can help individuals make lifestyle modifications to reduce their risk.
Stroke awareness involves recognizing the potential signs and symptoms of a stroke. Common stroke symptoms include sudden numbness or weakness in the face, arm, or leg, especially on one side of the body. Other symptoms may include confusion, trouble speaking or understanding speech, sudden difficulty walking or loss of balance, trouble seeing in one or both eyes, and a severe headache. If you or someone you know experiences any of these symptoms, it is crucial to act quickly and call emergency services.
| Risk Factors for Stroke | Prevention Strategies |
| Hypertension | Maintain a healthy blood pressure through regular check-ups and medication, if necessary. |
| Diabetes | Manage blood sugar levels through proper diet, exercise, and medication as prescribed by a healthcare professional. |
| High Cholesterol | Control cholesterol levels through a balanced diet, regular exercise, and medication, if recommended by a healthcare professional. |
| Smoking | Quit smoking to reduce the risk of stroke and other cardiovascular diseases. |
| Obesity | Maintain a healthy weight through a well-balanced diet and regular physical activity. |
| Poor Diet | Adopt a nutritious diet rich in fruits, vegetables, whole grains, and lean proteins. |
| Physical Inactivity | Engage in regular exercise and maintain an active lifestyle. |
| Excessive Alcohol Consumption | Limit alcohol intake to moderate levels as recommended by healthcare professionals. |
| Stress | Manage stress through relaxation techniques, regular exercise, and seeking support from friends, family, or healthcare professionals. |
By addressing these risk factors through lifestyle modifications and medical interventions, individuals can significantly reduce their risk of stroke. Regular health check-ups, blood pressure monitoring, and cholesterol and diabetes management are important for stroke prevention. Engaging in regular exercise, maintaining a healthy diet, avoiding smoking, and limiting alcohol consumption also play a vital role in reducing the risk of stroke.
The Unseen Connection
END
Priya’s tale is a reminder that in the relentless march of professional life, the heart’s whispers should not be ignored. For in its beat lies the rhythm of life itself, a melody that thrives not on the notes of achievement alone but on the harmony of health and happiness. The question that lingers is, will we listen?
This narrative serves as a gentle nudge, urging us to reflect on our choices. Are we ready to embrace the melody of a balanced life before the music fades?
Conclusion
In conclusion, it is crucial to be aware of the potential connections and risk factors for stroke awareness and heart attack prevention.
Recognizing the signs and symptoms of heart attacks and strokes is essential in order to seek immediate medical attention and minimize complications.
Additionally, taking proactive steps to reduce the risk of these life-threatening medical emergencies through lifestyle modifications, such as maintaining a healthy diet, exercising regularly, and managing stress, can greatly contribute to overall cardiovascular health.
Key Takeaways:
- Heart attacks and paralysis are distinct medical conditions with different causes.
- Recognizing the symptoms of a heart attack can help ensure immediate medical attention.
- Paralysis can result from damage to the nervous system and requires proper management.
- Understanding the risk factors for both heart attacks and paralysis is crucial for prevention.
- Prompt medical attention is essential for the best possible outcome in cases of heart attack or paralysis.
Q: What is the link between a stroke and a heart attack?
A: Both a stroke and a heart attack are cardiovascular events that can be caused by similar underlying issues such as thrombosis or coronary artery disease. These conditions can lead to reduced blood flow to the brain or heart, resulting in a stroke or heart attack respectively.
Q: What is the difference between a stroke and a heart attack?
A: A stroke occurs when the blood flow to the brain is disrupted, leading to potential brain damage, while a heart attack is caused by a blockage in one or more of the coronary arteries, interrupting blood flow to the heart muscle.
Q: What are the common symptoms of a stroke or a heart attack?
A: Common symptoms of a stroke include sudden numbness or weakness in the face, arm, or leg, especially on one side of the body, and difficulty speaking or understanding speech. Common symptoms of a heart attack include chest pain or discomfort, shortness of breath, and feeling lightheaded or dizzy.
Q: What can I do to reduce my risk of strokes and heart attacks?
A: To reduce your risk of strokes and heart attacks, it’s important to maintain a healthy lifestyle by eating a balanced diet, exercising regularly, controlling blood pressure and cholesterol levels, and avoiding smoking and excessive alcohol consumption.
Q: What kind of medical attention do strokes and heart attacks require?
A: Strokes and heart attacks are medical emergencies that require immediate medical attention. If you or someone around you shows signs of a stroke or heart attack, it’s crucial to seek medical help without delay to improve the chances of recovery.
Q: Is there a difference in how paralysis occurs in stroke cases and heart attacks?
A: Paralysis in stroke cases usually occurs on one side of the body, while in heart attack cases, paralysis is less common but can occur if there is extensive damage to the heart muscle.
Q: What are some of the vascular conditions that are linked to strokes and heart attacks?
A: Conditions such as thrombosis, coronary artery disease, and angina are examples of vascular ailments that can lead to strokes and heart attacks, highlighting the importance of managing these conditions to reduce the risk of cardiovascular events.
Q: How common are strokes and heart attacks in the U.S?
A: Strokes and heart attacks are leading causes of death in the U.S, with thousands of individuals suffering from stroke and heart attack every year. This emphasizes the importance of raising awareness about cardiovascular health and prevention measures.
Q: Can different types of strokes and heart attacks lead to permanent paralysis?
A: Yes, certain types of strokes and heart attacks can lead to permanent paralysis, especially if they cause extensive damage to the brain or spinal cord. Effective and immediate medical intervention can help minimize the risk of permanent paralysis.
Q: What is the importance of recognizing the signs and symptoms of strokes and heart attacks?
A: Recognizing the signs and symptoms of strokes and heart attacks is crucial as it enables quick identification and swift action, significantly improving the chances of recovery and reducing the potential long-term impact on the individual’s health.
Q: What is the link between heart attack and stroke?
A: Both heart attacks and strokes are caused by a lack of blood flow. A stroke occurs when the blood supply to the brain is interrupted, leading to brain tissue damage, while a heart attack happens when the blood flow to the heart is blocked, causing damage to the heart muscle. Both conditions are serious and require immediate medical attention.
Q: What are the symptoms of a heart attack?
A: Symptoms of a heart attack include chest pain or discomfort, shortness of breath, nausea, lightheadedness, and pain or discomfort in the arms, back, neck, jaw, or stomach. If you experience any of these symptoms, it’s crucial to seek emergency medical help immediately.
Q: What are the warning signs of a stroke?
A: The warning signs of a stroke include sudden numbness or weakness in the face, arm, or leg, especially on one side of the body, sudden confusion, trouble speaking or understanding, sudden trouble seeing in one or both eyes, sudden trouble walking, dizziness, loss of balance or coordination, and sudden severe headache with no known cause. If you or someone else experiences any of these symptoms, it’s essential to call for help immediately.
Q: Can a stroke cause paralysis?
A: Yes, a stroke can cause paralysis, typically on one side of the body. Depending on the area of the brain affected by the stroke, a person may experience varying degrees of paralysis, ranging from mild weakness to complete inability to move. Seeking immediate medical help can reduce the risk of long-term paralysis and improve recovery outcomes.
Q: What should I do if I suspect someone is having a stroke?
A: If you suspect someone is having a stroke, it’s crucial to act fast. Call emergency medical services immediately and note the time when the symptoms began. Quick medical intervention can help preserve brain function and improve the chances of recovery.
Q: How can I reduce my risk of heart attack and stroke?
A: You can reduce your risk of heart attack and stroke by maintaining a healthy lifestyle, including regular exercise, a balanced diet, managing stress, monitoring blood pressure and cholesterol levels, and avoiding smoking and excessive alcohol consumption. Regular health check-ups and preventive care can also help identify and address risk factors for these conditions.
Q: What’s the difference between a heart attack and a stroke?
A: A heart attack, or myocardial infarction, occurs when the blood flow to the heart is blocked, causing damage to the heart muscle. On the other hand, a stroke, also known as a cerebrovascular accident, happens when the blood supply to the brain is interrupted, leading to brain tissue damage. While both are medical emergencies, they affect different organs in the body.
Q: Can a heart attack also cause paralysis?
A: While a heart attack is not typically associated with paralysis, in some cases, complications such as arrhythmia or autonomic dysreflexia may lead to temporary or long-term paralysis. Any unexpected inability to move or other concerning symptoms during or after a heart attack should prompt immediate medical attention.
Q: How does a stroke affect the ability to move?
A: A stroke can affect the ability to move by causing paralysis or weakness in one side of the body, known as hemiplegia or hemiparesis. The area of the brain affected by the stroke determines the extent and specifics of the movement impairment. Rehabilitation and medical treatment are crucial in improving movement and function after a stroke.
Q: Can both heart attack and stroke lead to damage due to a lack of oxygen?
A: Yes, both heart attack and stroke can lead to damage to the affected organs, such as the heart or brain, due to a lack of oxygen and nutrients. This damage can be minimized with prompt medical intervention and treatment to restore blood flow and oxygen supply to the affected tissues.
