When it comes to treating heart failure and heart attack, the impact of oxygen flow rate cannot be ignored. Oxygen therapy plays a crucial role in the efficacy of these treatments, and it has been extensively studied by reputable sources such as the American College of Cardiology Foundation/American Heart Association Task Force, JAMA, and N Engl J Med.
It is well-established that the flow rate of oxygen has a significant effect on the outcomes of heart failure and heart attack treatments. The right oxygen flow rate can make a difference in the recovery and well-being of patients.
Are you aware of how oxygen flow rate affects the effectiveness of heart treatment? Let’s explore this topic in detail and understand the various factors at play.
Key Takeaways:
- Oxygen flow rate is a critical factor in the efficacy of heart failure and heart attack treatments.
- The right oxygen flow rate can significantly improve patient outcomes.
- Reputable sources such as the American College of Cardiology Foundation/American Heart Association Task Force, JAMA, and N Engl J Med have extensively studied the impact of oxygen flow rate on heart treatment efficacy.
- Understanding the effects of oxygen flow rate is crucial for healthcare professionals to provide optimal care.
- Further research is needed to determine the optimal oxygen flow rate for different heart conditions.
Oxygen Therapy for Heart Failure and Heart Attack
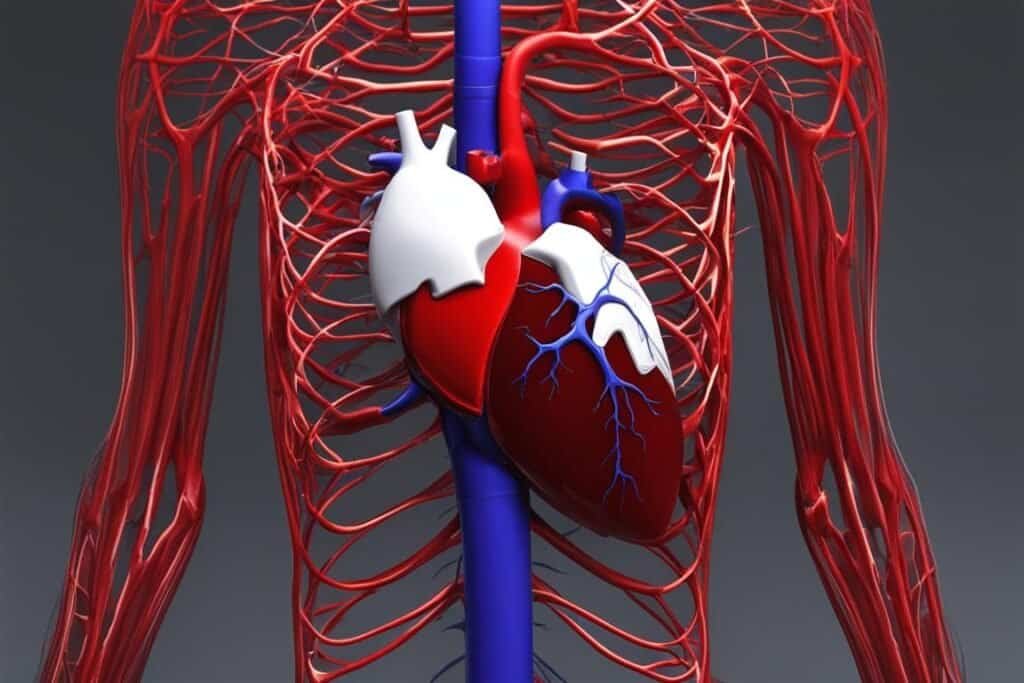
Oxygen therapy plays a crucial role in the treatment of heart failure and heart attack. The flow rate of oxygen administration directly impacts the effectiveness of this treatment. Studies have shown that high-flow oxygen therapy through nasal cannula (HFNC) can significantly reduce intubation rates and mortality rates in patients with acute respiratory failure. In fact, HFNC therapy has been recommended as the initial choice of oxygen therapy for selected patients with heart failure.
High-flow oxygen therapy delivers a higher flow rate of oxygen compared to standard oxygen therapy. This increased flow rate enables better oxygenation of the blood and improves the functioning of the heart. By providing a higher concentration of oxygen, HFNC therapy can enhance the oxygen delivery to the tissues, thereby improving heart function.
One of the key advantages of HFNC therapy is its ability to maintain positive pressure in the airways, which helps prevent airway collapse and improves oxygenation. Additionally, the high-flow rate of oxygen delivered through HFNC therapy can facilitate the removal of carbon dioxide from the body, further improving respiratory function.
Research has also shown that HFNC therapy has a positive impact on physiological responses in patients with heart failure and heart attack. This therapy can effectively improve mean arterial pressure, heart rate, and oxygen saturation levels. By optimizing these physiological parameters, HFNC therapy contributes to better heart function and overall treatment efficacy.
Moreover, a comparative analysis between HFNC therapy and traditional methods of oxygen therapy, such as endotracheal intubation, has shown comparable in-hospital clinical outcomes. HFNC therapy has demonstrated a high success rate in avoiding intubation, resulting in improved patient comfort and reduced risks associated with invasive procedures.
Overall, the use of high-flow oxygen therapy through nasal cannula is a promising approach in the treatment of heart failure and heart attack. Its ability to optimize oxygen delivery, maintain positive airway pressure, and improve physiological responses makes it an effective and preferred choice of oxygen therapy for selected patients. Further research on the optimal flow rates and long-term benefits of HFNC therapy is essential to enhance heart treatment efficacy and ensure better patient outcomes.
| Benefits of HFNC Therapy for Heart Failure and Heart Attack | Traditional Methods of Oxygen Therapy |
|---|---|
|
|
Physiological Responses to High-Flow Oxygen Therapy
When you undergo high-flow oxygen therapy through a nasal cannula (HFNC), your body experiences various physiological responses that contribute to its effectiveness in treating heart failure and heart attack. These responses include changes in mean arterial pressure, heart rate, respiratory rate, and oxygen saturation.
The initial gas flow and fraction of inspired oxygen concentration (FiO2) during HFNC therapy are adjusted to achieve a target oxygen saturation level of over 90%. This ensures that your body receives an adequate supply of oxygen to support its functioning.
Studies have demonstrated that HFNC therapy is effective in improving oxygen saturation levels, comparable to traditional methods of oxygen therapy. This makes it a viable treatment option for patients with heart failure and heart attack.

Comparison of HFNC and Intubation in AHF Patients
When it comes to treating acute heart failure (AHF), the choice between high-flow oxygen therapy through nasal cannula (HFNC) and endotracheal intubation is an important consideration. A retrospective cohort analysis compared the outcomes of patients who received HFNC with those who underwent intubation, shedding light on the efficacy of these treatment options.
The study found that HFNC therapy resulted in similar improvements in oxygen saturation levels compared to intubation therapy. Patients receiving HFNC showed significant physiological responses, such as improved mean arterial pressure, heart rate, and oxygen saturation. These responses indicate that HFNC therapy effectively supports cardiac function and oxygenation in AHF patients.
Furthermore, in-hospital clinical outcomes for both HFNC and intubation therapy were comparable. This suggests that HFNC therapy can provide effective treatment for AHF patients without the need for invasive intubation procedures.
The success rate of HFNC therapy in avoiding intubation was high, indicating that it can serve as an alternative to intubation in certain cases. HFNC therapy offers numerous benefits, including improved patient comfort, reduced risk of complications associated with intubation, and better preservation of airway protective reflexes.
| Comparison | HFNC Therapy | Intubation |
|---|---|---|
| Oxygen Saturation | Similar improvements | N/A |
| Physiological Responses | Positive changes in mean arterial pressure, heart rate, and oxygen saturation | N/A |
| In-Hospital Clinical Outcomes | Comparable outcomes | N/A |
| Intubation Avoidance Success | High success rate | N/A |
Overall, the comparison between HFNC therapy and intubation in AHF patients demonstrates that HFNC therapy is a viable treatment option with similar physiological responses and in-hospital clinical outcomes. Its success in avoiding intubation further supports its potential as a preferred non-invasive approach to managing AHF patients. However, it’s important to note that the choice of treatment should be individualized based on the patient’s condition and the healthcare provider’s assessment.
Effects of Oxygen Flow Rate on Coronary Blood Flow
Supplemental oxygen administration during cardiac catheterization procedures has been found to have an impact on coronary blood flow. Research studies have shown that hyperoxia, characterized by high oxygen concentrations, can cause changes in coronary blood flow, suggesting that the oxygen flow rate may play a role in cardiac function. These findings have important implications in the management of patients with ischemic heart disease.
In addition to its effects on coronary blood flow, hyperoxia has also been studied for its impact on regional blood flow, oxygen consumption, and central circulation in patients with ischemic heart disease. By understanding how changes in oxygen flow rate can influence these physiological factors, healthcare professionals can better assess and optimize treatment strategies for patients.
| Effect | Impact |
|---|---|
| Coronary Blood Flow | Hyperoxia can cause changes in coronary blood flow. |
| Regional Blood Flow | The effects of hyperoxia on regional blood flow have been studied in ischemic heart disease. |
| Oxygen Consumption | Research has examined the influence of hyperoxia on oxygen consumption in patients with ischemic heart disease. |
| Central Circulation | The effects of hyperoxia on central circulation have been investigated in the context of ischemic heart disease. |
Understanding the effects of oxygen flow rate on coronary blood flow and related physiological responses is essential for optimizing cardiac catheterization procedures and improving outcomes for patients with ischemic heart disease. Further research in this area will continue to enhance our understanding of the intricate relationship between oxygen flow and cardiac function.
Oxygen Therapy in Myocardial Infarction
The use of oxygen therapy in the treatment of myocardial infarction (MI), commonly known as a heart attack, has been a topic of debate in the medical community. Research suggests that the routine use of oxygen may not always be beneficial and can sometimes have adverse effects on patients with MI.
Systematic reviews and analyses from the Cochrane database have found that the administration of oxygen in the treatment of MI does not result in significant improvements in clinical outcomes. While oxygen therapy is commonly used to increase oxygen levels in the blood and alleviate symptoms of ischemia, studies have not consistently shown a positive impact on patient outcomes.
Although providing supplemental oxygen may seem logical, it is important to note that excess oxygen administration can potentially lead to oxidative stress and vasoconstriction in the coronary arteries, thus compromising blood flow to the heart muscle. Striking the right balance in oxygen delivery is crucial to avoid potential harm and maximize clinical benefits.
As a result, current guidelines from organizations such as the American Heart Association do not recommend routine oxygen administration in the absence of hypoxemia (low oxygen levels in the blood). Instead, oxygen therapy is reserved for patients with symptoms of low oxygen, such as chest pain, shortness of breath, or unstable vital signs.
Further research is needed to determine the appropriate use of oxygen therapy in myocardial infarction and to identify specific subsets of patients who may benefit from this intervention. By understanding the potential risks and limitations of oxygen therapy, healthcare professionals can make informed decisions to optimize patient care and improve clinical outcomes in the management of myocardial infarction.
| Pros of Oxygen Therapy in MI | Cons of Oxygen Therapy in MI |
|---|---|
|
|
*Studies have not consistently shown a positive impact on patient outcomes.
Conclusion
The impact of oxygen flow rate on heart treatment efficacy is a crucial consideration in the medical field. Studies have consistently demonstrated that high-flow oxygen therapy through nasal cannula (HFNC) can effectively improve oxygen saturation levels and yield comparable clinical outcomes to intubation therapy for patients with acute heart failure. The physiological responses to HFNC therapy, including changes in mean arterial pressure, heart rate, and oxygen saturation, are similar to those observed with traditional methods of oxygen therapy. However, further research is needed to determine the optimal oxygen flow rate for achieving optimal heart treatment efficacy.
Understanding the relationship between oxygen flow rate and heart treatment efficacy is essential for improving patient outcomes. By optimizing the oxygen flow rate, healthcare professionals can ensure that patients receive the most appropriate level of oxygenation to support their cardiovascular function. This knowledge can guide the selection of oxygen therapy strategies, such as HFNC, which have shown promising results in maintaining oxygen saturation levels and avoiding intubation in patients with acute heart failure.
Clinical outcomes play a significant role in assessing the effectiveness of heart treatment approaches. The ability of HFNC therapy to achieve comparable clinical outcomes to intubation therapy in patients with acute heart failure is encouraging. By recognizing the physiological responses to HFNC therapy and understanding the impact of oxygen flow rate on heart treatment efficacy, healthcare providers can implement evidence-based strategies to optimize patient care and improve outcomes for individuals with heart conditions.