Introduction
🌟 Did you know that recovering from a heart attack is not just about healing the heart, but also about arming it for the future? For Indian professionals in their 30s, 40s, and 50s, understanding the medications prescribed after a heart attack is like equipping a soldier for battle. These medications are crucial in not only aiding recovery but also in fortifying the heart against future threats.
In this blog, we delve into the various medications commonly prescribed after a heart attack. From aspirin, which acts like a peacekeeper preventing blood clots, to beta blockers that help calm the heart’s rhythm, each medication plays a unique role in your heart’s recovery journey. We’ll explore how these medicines work together to reduce the risk of a subsequent heart attack and improve overall heart health.
With simple, easy-to-understand explanations, this blog is designed to demystify the complex world of post-heart attack medications. It’s a guide to help you navigate this crucial phase of recovery, ensuring that your heart, much like a well-guarded fortress, remains strong and protected.
Diagnosing a Heart Attack
Diagnosing a heart attack involves a series of tests and procedures to accurately assess your heart health and detect any signs or symptoms of a potential heart attack. These diagnostic measures help healthcare professionals make informed decisions about your treatment plan.
Heart Attack Symptoms
Before diving into the diagnostic procedures, it’s crucial to be aware of the common symptoms of a heart attack. These symptoms may include:
- Chest pain or discomfort
- Shortness of breath
- Pain radiating to the arm, shoulder, jaw, neck, or back
- Nausea or indigestion
- Lightheadedness or fainting
Heart Health Screening
When you visit a healthcare professional with symptoms indicating a potential heart attack, they will conduct a thorough heart health screening. This screening helps determine if you have any underlying heart conditions or risk factors that may contribute to a heart attack. The screening may include:
- Discussion of your medical history and symptoms
- Physical examination
- Assessment of cardiovascular risk factors such as family history, smoking history, high blood pressure, high cholesterol, and diabetes
Heart Attack Tests
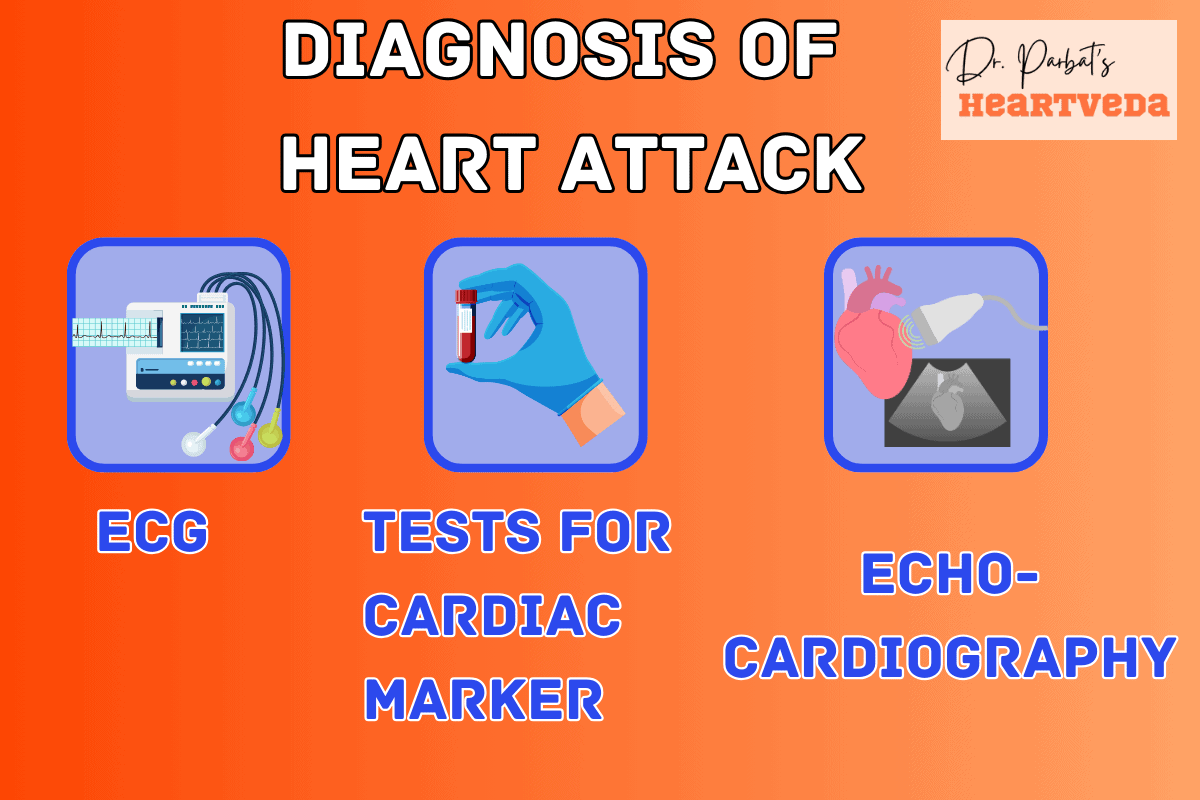
To confirm or rule out a heart attack, your healthcare provider may recommend the following tests:
| Test | Purpose |
| Electrocardiogram (ECG or EKG) | Measures electrical signals in the heart to detect abnormalities or signs of a heart attack |
| Blood tests | Check for specific enzymes or proteins released during a heart attack to assess heart damage |
| Chest X-ray | Evaluates the condition of the heart and lungs |
| Echocardiogram | Uses sound waves to create images of the heart, assessing its function and potential damage |
| Coronary catheterization (angiogram) | Inserts a dye into the arteries to identify blockages or narrowing in the coronary arteries |
| Cardiac CT or MRI | Provides detailed images of the heart to detect any structural abnormalities or assess heart function |
Based on the results of these tests, your healthcare provider will be able to diagnose whether you have experienced a heart attack or if your symptoms are due to another condition. Early and accurate diagnosis is crucial for timely treatment and minimizing potential complications.
Foundations of Survival: The Architect’s Journey
Part -1
In the heart of Chennai, where the sun paints the sky in hues of gold every morning, lived Vikram, a 48-year-old architect. His life was a canvas of creativity, designing skyscrapers that reached for the clouds, yet his own health was a blueprint he often neglected.
Vikram’s home was a reflection of his love for aesthetics, shared with his wife, a school teacher, and their teenage daughter. Despite his keen emotional intelligence, enabling him to empathize with clients and colleagues alike, Vikram viewed his health through a lens of denial, prioritizing deadlines over doctor’s appointments.
Heart Attack Medications
Medications play a crucial role in treating and preventing heart attacks. If you have experienced a heart attack or are at high risk for one, your doctor may prescribe certain medications to help manage your condition and reduce the risk of future heart attacks.
Aspirin
One commonly used medication is aspirin. Aspirin helps reduce blood clotting, which can be a significant factor in heart attacks. Taking a daily low-dose aspirin can help prevent blood clots from forming and decrease the risk of heart attack.
Clot Busters
In some cases, clot busters may be used to break up blood clots that are causing a heart attack. These medications work quickly to dissolve the clot and restore blood flow to the heart.
Blood-Thinning Medicines
Blood-thinning medicines, such as heparin, can also help prevent blood clots from forming. These medications are often prescribed to individuals who are at high risk for heart attack or have a history of blood clots.
Nitroglycerin
Nitroglycerin is a medication that improves blood flow by dilating the blood vessels. It is commonly used to relieve chest pain or discomfort caused by a heart attack and can also help prevent future episodes.
Morphine
Morphine may be given to individuals experiencing severe chest pain during a heart attack. It helps relieve pain and reduce anxiety, allowing the heart to work more efficiently.
Beta Blockers
Beta blockers are medications that slow the heartbeat and lower blood pressure. They help reduce the workload on the heart and can be prescribed to individuals who have had a heart attack or are at risk for one.
ACE Inhibitors
ACE inhibitors are another type of medication that can be prescribed after a heart attack. They help lower blood pressure and reduce strain on the heart, preventing further damage and improving heart function.
Statins
Statins are commonly prescribed to lower cholesterol levels. High cholesterol is a major risk factor for heart attacks, so taking statins can help reduce the risk. These medications work by blocking an enzyme that produces cholesterol in the liver, leading to lower cholesterol levels in the blood.
It’s important to note that these medications may have specific dosages and potential side effects associated with them. It’s essential to follow your doctor’s instructions and report any unusual symptoms or concerns while taking these medications.
Role of Drugs in Secondary Prevention of Heart Attack
| Drug Group | Common Drugs | Function and Role in Secondary Prevention |
| Antiplatelet Therapy | Aspirin | – Prevents blood platelets from clumping, reducing blood clot risk. – Lowers risk of another heart attack and heart-related issues. – Recommended for long-term use after a heart attack. |
| β-Adrenoceptor Blockers | Metoprolol, Atenolol | – Slows heart rate and lowers blood pressure, reducing heart workload. – Associated with lower death rates, reduced heart attack size, and fewer rhythm problems. – Beneficial in long-term use. |
| ACE Inhibitors | Lisinopril, Ramipril | – Relaxes blood vessels, easing heart’s workload. – Particularly beneficial for patients with heart failure or reduced heart function post-heart attack. – Drug choice depends on patient and clinical factors. |
| Cholesterol-Lowering Drugs (Statins) | Atorvastatin, Simvastatin | – Reduces bad cholesterol, preventing arterial clogging. – Significantly reduces future heart attack risk and death in high cholesterol patients. – Watch for side effects like muscle pain, small diabetes risk. |
| Calcium Channel Blockers | Amlodipine, Diltiazem | – Relaxes blood vessel muscles. – Use in post-heart attacks is controversial and not routinely recommended. |
| Anti-Arrhythmic Drugs | Amiodarone | – Controls abnormal heart rhythms. – Not widely recommended post-heart attack, but beneficial in high-risk groups with heart failure or arrhythmias. |
| Anticoagulants | Warfarin | – Prevents blood clots, reducing heart attack/stroke risk. – Effective but increased bleeding risk. – Especially beneficial in high-risk groups like those with atrial fibrillation or severe heart failure. |
Foundations of Survival: The Architect’s Journey
Part – 2
His daily routine was a marathon of meetings, site visits, and late-night drafting sessions. This relentless pursuit of architectural excellence left little room for exercise or proper nutrition, a lifestyle choice Vikram justified with the age-old adage, “I’ll rest when I retire.”
The consequence of his neglect came unannounced, a heart attack that struck with the suddenness of a monsoon storm. It was a wake-up call that echoed through the corridors of his meticulously designed life, leaving him vulnerable in a hospital bed, surrounded by the sterile precision he so often applied to his projects.
Vikram’s darkest moment wasn’t the physical pain of the heart attack but the realization of its implications. The thought of his designs remaining uncompleted, of his daughter’s milestones witnessed only in photographs, and of his wife navigating the future alone was a prospect more terrifying than any client critique.
Surgical and Other Procedures
When it comes to treating a heart attack, surgical interventions or procedures may be necessary. These procedures aim to restore blood flow to the heart and improve overall heart health. Here are some of the common heart attack treatment procedures:
Coronary Angioplasty and Stenting
In this procedure, a thin tube called a catheter is inserted into a blocked coronary artery. A balloon attached to the catheter is inflated to open up the narrowed artery, allowing for improved blood flow. In some cases, a stent, which is a small mesh tube, may be placed to support the artery and keep it open.
Coronary Artery Bypass Grafting (CABG)
CABG surgery is performed when the coronary arteries are severely blocked or damaged. The surgeon uses a healthy blood vessel from another part of your body, such as the chest or leg, to create a bypass around the blocked artery. This creates a new path for blood to flow freely to the heart, bypassing the blockage.
Cardiac Rehabilitation
Cardiac rehabilitation is a comprehensive program that helps individuals recover from a heart attack and improve their heart health. It involves a combination of exercise, education, and lifestyle modifications. The program is designed to help patients regain strength, reduce the risk of future heart problems, and improve overall cardiovascular fitness.
| Treatment Procedure | Description |
| Coronary Angioplasty and Stenting | A procedure to open blocked coronary arteries using a balloon and placing a stent to keep the artery open. |
| Coronary Artery Bypass Grafting (CABG) | Surgical procedure to create new paths for blood flow by bypassing blocked coronary arteries. |
| Cardiac Rehabilitation | Comprehensive program involving exercise, education, and lifestyle modifications to aid in recovery and improve heart health. |
Self-Care for Heart Health
Taking care of your heart is vital for maintaining overall health and preventing heart attacks. By making healthy lifestyle choices and incorporating certain habits into your daily routine, you can significantly reduce the risk of heart disease and improve your heart health.
Exercise Regularly
Engaging in regular physical activity is one of the best ways to keep your heart healthy. Aim for at least 150 minutes of moderate aerobic exercise or 75 minutes of vigorous aerobic exercise each week. Some activities you can try include brisk walking, jogging, cycling, swimming, or dancing. Consult with your healthcare provider before starting any new exercise regimen.
Maintain a Balanced Diet
Eating a heart-healthy diet is essential for preventing heart disease and reducing the risk of heart attacks. Focus on consuming a variety of fruits, vegetables, whole grains, lean proteins, and healthy fats. Limit your intake of saturated and trans fats, sodium, and added sugars. Include foods rich in omega-3 fatty acids, such as fatty fish like salmon or trout, walnuts, and flaxseeds.
Manage Weight
Maintaining a healthy weight is crucial for heart health. Excess weight can strain your heart and increase the risk of developing heart disease. Create a balanced eating plan and incorporate regular physical activity to achieve and maintain a healthy weight. Seek guidance from a healthcare professional or registered dietitian for personalized weight management strategies.
Quit Smoking
Smoking is a major risk factor for heart disease and can lead to heart attacks. If you smoke, it is important to quit as soon as possible. Seek support from healthcare professionals, quit smoking programs, or support groups to assist you in your journey towards becoming smoke-free. The benefits of quitting smoking are significant for your heart and overall health.
Moderate Alcohol Intake
While moderate alcohol consumption may have some health benefits, excessive drinking can negatively impact your heart health. If you choose to drink, do so in moderation. The recommended limits are no more than one drink per day for women and no more than two drinks per day for men. Be mindful of your alcohol consumption and seek professional guidance if you have concerns.
Schedule Regular Checkups
Regular checkups with your healthcare provider are essential for maintaining heart health. They can help monitor your blood pressure, cholesterol levels, and overall cardiovascular health. Discuss any concerns, symptoms, or changes in your health with your healthcare provider. Routine screenings and early detection of any issues can significantly improve your heart health outcomes.
Manage Blood Pressure
High blood pressure is a significant risk factor for heart attacks. Take steps to keep your blood pressure within a healthy range by following your healthcare provider’s recommendations. This may include lifestyle modifications, such as a heart-healthy diet, regular exercise, stress reduction techniques, and medication, if prescribed.
Control Cholesterol Levels
High cholesterol levels can contribute to the development of heart disease. Follow a heart-healthy diet low in saturated and trans fats, engage in regular physical activity, and take medications if prescribed by your healthcare provider to manage your cholesterol levels. Regular monitoring and management of cholesterol are key to preventing heart attacks.
Reduce Stress
Chronic stress can negatively impact heart health. Find healthy ways to manage and reduce stress levels, such as engaging in relaxation techniques like deep breathing exercises, meditation, or yoga. Incorporate stress-reducing activities into your daily routine to promote overall well-being and improve heart health.
Tips for a Heart-Healthy Lifestyle
| Lifestyle Habits | Description |
| Exercise regularly | Aim for at least 150 minutes of moderate aerobic exercise or 75 minutes of vigorous aerobic exercise each week. |
| Eat a balanced diet | Include a variety of fruits, vegetables, whole grains, lean proteins, and healthy fats in your diet. Limit saturated and trans fats, sodium, and added sugars. |
| Maintain a healthy weight | Create a balanced eating plan and engage in regular physical activity to achieve and maintain a healthy weight. |
| Quit smoking | Seek support to quit smoking and improve your heart health. |
| Moderate alcohol intake | Drink alcohol in moderation, following the recommended guidelines. |
| Schedule regular checkups | Visit your healthcare provider regularly for checkups and screenings to monitor your heart health. |
| Manage blood pressure | Follow your healthcare provider’s recommendations to keep your blood pressure within a healthy range. |
| Control cholesterol levels | Follow a heart-healthy diet, exercise regularly, and take prescribed medication to manage your cholesterol levels. |
| Reduce stress | Practice stress reduction techniques, such as deep breathing exercises, meditation, or yoga. |
Foundations of Survival: The Architect’s Journey
Part – 3
The path to recovery introduced Vikram to a regimen of medications, a cocktail of science designed to mend his heart and prevent future attacks. Dr. Nair, his cardiologist, emphasized the importance of adherence to these medications, likening them to the foundational elements of a building that, if ignored, could compromise the entire structure.
Vikram’s journey from denial to acceptance was marked by his commitment to his health. He began to view his medications as non-negotiable elements of his day, as essential as the blueprints that guided his creations. With the support of his family, he slowly rebuilt his life, incorporating exercise and a balanced diet into his routine.
His story became a message of caution and hope for his peers, a reminder that the brilliance of their creations was grounded in their health. Vikram shared his experience openly, advocating for the critical role of medication adherence post-heart attack, not just for survival but for the quality of life thereafter.
Coping and Support
Coping with the emotional aftermath of a heart attack can be challenging. It is important to seek support to help alleviate anxiety and depression during the recovery process.
Here are some ways you can find the emotional support you need:
- Talk to healthcare providers: Openly discuss your emotions and concerns with your healthcare providers. They can offer guidance, advice, and recommend resources for support.
- Lean on family and friends: Reach out to your loved ones for understanding and comfort. They can provide a listening ear and offer emotional support during this time.
- Join heart attack support groups: Connecting with others who have experienced a heart attack can be incredibly helpful. Support groups provide a safe space to share experiences, exchange coping strategies, and offer mutual support.
- Consider mental health care: If you are struggling with depression or anxiety after a heart attack, seeking professional mental health care can be beneficial. Therapists or counselors can help you navigate the emotional challenges and provide coping mechanisms.
Remember that everyone’s recovery journey is unique, and it is important to prioritize your mental well-being as you heal physically. Taking advantage of cardiac rehabilitation programs can also assist in addressing any emotional challenges and improving overall well-being.
When to Resume Sexual Activity after a Heart Attack
Resuming sexual activity after a heart attack is a common concern. Most individuals can safely engage in sexual activity after recovery, but it’s essential to consult with a healthcare provider. Some heart medications may affect sexual function, and discussing any concerns or issues with a healthcare provider is recommended.
Preparing for Your Appointment
Being prepared for your medical appointments can help ensure productive discussions with your healthcare provider. It’s important to gather relevant information and ask the right questions to make the most of your appointment. Here are some tips to help you prepare:
1. Assess your cardiovascular risk
Prior to your appointment, take some time to evaluate your cardiovascular risk factors. Consider factors such as your age, family history of heart disease, smoking habits, and existing medical conditions. This information will help your healthcare provider assess your risk and develop a personalized prevention plan.
2. Monitor your cholesterol and blood pressure levels
Knowing your cholesterol and blood pressure levels is crucial for evaluating your heart health. If you have recent test results, bring them with you to the appointment. If not, discuss with your healthcare provider whether you should have these tests done during your visit.
3. Prepare a list of questions
Before your appointment, make a list of questions you want to ask your healthcare provider. This will ensure that your concerns are addressed and you leave the appointment with a clear understanding of your heart attack prevention and treatment plan. Consider asking about the benefits and risks of statins, any lifestyle changes you should make, and how to manage your risk factors effectively.
4. Review your medications and supplements
Make a list of all the medications and supplements you are currently taking. This includes prescription drugs, over-the-counter medications, and any herbal supplements. Bring this list with you to your appointment, as it will help your healthcare provider assess any potential drug interactions or side effects.
5. Stay informed
Take initiative in educating yourself about heart attack prevention. Stay updated on the latest research and recommendations, as well as common symptoms and warning signs. This knowledge will empower you to make informed decisions about your heart health.
An informed patient is an empowered patient. By being prepared for your appointment, you can actively participate in your heart attack prevention and treatment journey.
Statins for Heart Attack Prevention
Statins are a commonly prescribed medication for reducing cholesterol levels and lowering the risk of heart attacks and strokes. They are particularly recommended for individuals who have certain risk factors such as high cholesterol, diabetes, high blood pressure, or are smokers. Statins work by blocking the enzyme in the liver responsible for producing cholesterol, thus reducing cholesterol levels in the blood.
Lowering cholesterol is crucial for managing high cholesterol levels and preventing the buildup of plaque in the arteries. By reducing cholesterol, statins help to improve blood flow and lower the risk of heart attacks.
Statins offer several benefits for heart attack prevention:
- Reduced cholesterol levels: By lowering cholesterol levels, statins help to manage high cholesterol and prevent the accumulation of plaque in the arteries.
- Lower heart attack risk: Statins have been shown to significantly reduce the risk of heart attacks in individuals at higher risk, including those with diabetes, high blood pressure, or smokers.
- Improved heart health: By improving blood flow and reducing cholesterol, statins promote overall heart health and reduce the risk of cardiovascular events.
However, it’s important to be aware of the potential risks and side effects of statins:
- Muscle pain and weakness: Some individuals may experience muscle-related side effects such as pain, weakness, or inflammation while taking statins. It’s essential to report any unusual symptoms to your healthcare provider.
- Liver damage: In rare cases, statins can cause liver damage. Regular liver function tests are typically recommended for individuals taking statins to monitor liver health.
- Digestive issues: Statins may cause digestive problems such as nausea, diarrhea, or constipation in some individuals. These side effects are usually temporary and improve over time.
- Interaction with other medications: Statins may interact with other medications, including certain antibiotics and drugs used to treat HIV or hepatitis. It’s important to inform your healthcare provider about all the medications you are taking.
It’s crucial to discuss the benefits, risks, and potential side effects of statin therapy with your healthcare provider. They can assess your individual risk factors, cholesterol levels, and determine whether statins are the appropriate choice for heart attack prevention in your case.
Other Heart Attack Medications
In addition to statins, there are several other medications that may be prescribed to prevent heart attacks and manage related conditions. These medications can provide various benefits in reducing the risk of heart attack, but it’s important to be aware of their potential risks and side effects. It is crucial to discuss these options with your healthcare provider to determine the most appropriate medication for your specific circumstances and medical history.
- ACE inhibitors: ACE inhibitors, such as Lisinopril and Ramipril, are commonly prescribed to treat high blood pressure and manage heart failure. They work by helping to relax blood vessels and lower blood pressure, reducing the workload on the heart.
- Aspirin therapy: Aspirin is often recommended as a preventative measure for individuals at high risk of heart attack. It helps to prevent blood clot formation by inhibiting platelet aggregation, thereby reducing the risk of blockages in the arteries.
- Beta blockers: Beta blockers, such as Metoprolol and Atenolol, are commonly prescribed to reduce blood pressure and heart rate. They help to decrease the workload on the heart and can be beneficial for individuals with a history of heart attack or heart failure.
- Antiplatelets: Antiplatelet medications, such as Clopidogrel and Ticagrelor, are used to prevent blood clot formation. They work by inhibiting platelet activation and aggregation, reducing the risk of artery blockage and subsequent heart attack.
- Diuretics: Diuretics, such as Furosemide and Hydrochlorothiazide, are commonly prescribed to manage high blood pressure and reduce fluid retention. They help to lower blood volume, easing the strain on the heart.
- Blood thinners: Blood thinners, such as Warfarin and Apixaban, are prescribed to prevent blood clot formation in individuals at high risk of heart attack or stroke. They inhibit the clotting factors in the blood, reducing the likelihood of blockages in the arteries.
While these medications can be beneficial in preventing heart attacks and managing related conditions, they do come with risks and potential side effects. It’s important to work closely with your healthcare provider to monitor your response to these medications and discuss any concerns or symptoms that arise.
Each medication may have different interactions, contraindications, and possible side effects. Your healthcare provider will guide you in determining the best medication option, dosage, and duration of treatment based on your individual needs and medical history.
Lifestyle Changes for Heart Attack Prevention
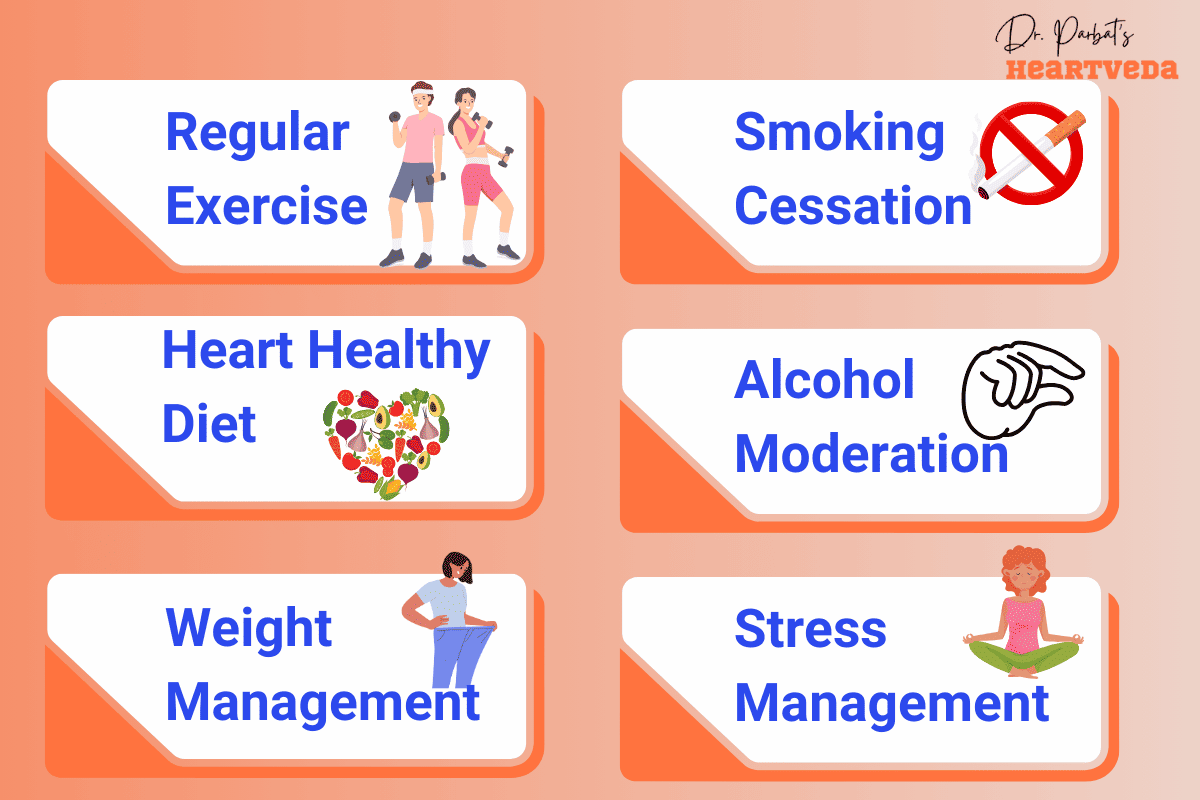
Along with medication, making lifestyle changes is essential for preventing heart attacks. By adopting a heart-healthy lifestyle, you can significantly reduce your risk of experiencing a heart attack and improve your overall heart health.
Exercise Recommendations
Regular exercise is a key component of heart attack prevention. Aim for at least 150 minutes of moderate-intensity aerobic activity or 75 minutes of vigorous-intensity aerobic activity per week. Some examples include brisk walking, jogging, cycling, swimming, or dancing. Remember to consult with your healthcare provider before starting any exercise program.
Heart-Healthy Diet
Eating a nutritious, heart-healthy diet is crucial. Focus on consuming fruits, vegetables, whole grains, lean proteins, and foods low in saturated fats, trans fats, cholesterol, and sodium. Incorporate omega-3 fatty acids found in fish, walnuts, and flaxseeds for added heart protection. Limit your intake of sugary beverages, processed foods, and excessive salt.
Weight Management
Maintaining a healthy weight is important for heart health. If you’re overweight or obese, aim to lose weight through a combination of healthy eating and regular physical activity. Consult with a registered dietitian or healthcare provider to develop a personalized plan.
Smoking Cessation
Quit smoking if you’re a smoker. Smoking is a major risk factor for heart attacks and a range of other health issues. Seek support from healthcare professionals, nicotine replacement therapy, or smoking cessation programs to increase your chances of success.
Alcohol Moderation
Limit your alcohol consumption to moderate levels. For men, this means up to two drinks per day, and for women, it’s up to one drink per day. Excessive alcohol consumption can increase your risk of heart disease and other health problems.
Stress Reduction
Manage stress levels through relaxation techniques like deep breathing exercises, meditation, yoga, or engaging in hobbies you enjoy. Prioritize self-care and make time for activities that help you unwind and relax.
“Preventing heart attacks requires a holistic approach. By adopting a heart-healthy lifestyle, incorporating regular exercise, following a nutritious diet, managing your weight, quitting smoking, moderating alcohol intake, and reducing stress, you can significantly reduce your risk of heart attack and improve overall heart health.”
| Lifestyle Changes | Benefits |
| Regular Exercise | – Increased cardiovascular fitness- Lower blood pressure- Improved cholesterol levels- Weight management |
| Heart-Healthy Diet | – Reduced risk of heart disease- Lower cholesterol levels- Improved blood sugar control- Weight management |
| Weight Management | – Lower risk of heart disease- Improved blood pressure and cholesterol levels- Reduced strain on the heart |
| Smoking Cessation | – Lower risk of heart attack and other smoking-related diseases- Improved lung function and overall health |
| Alcohol Moderation | – Lower risk of heart disease and liver damage- Improved overall health and well-being |
| Stress Reduction | – Lower blood pressure and heart rate- Improved mental well-being- Better overall quality of life |
Foundations of Survival: The Architect’s Journey
End
As he returned to his drawing board, Vikram pondered a question that resonated beyond the realms of architecture: “What is the value of our achievements if we’re not around to witness their impact?” It was an invitation to his fellow professionals to prioritize their health, ensuring their legacy would be enjoyed for generations to come.
The message was clear: adherence to prescribed medications post-heart attack is not just a recommendation but a lifeline, a foundation upon which the future is built, ensuring that the heart, much like the structures they designed, stood the test of time.
Conclusion
In conclusion, preventing heart attacks requires a comprehensive approach that incorporates medication, lifestyle changes, and regular medical checkups. By taking proactive steps to reduce risk factors and maintain a healthy lifestyle, you can significantly decrease your chances of experiencing a heart attack and improve your overall heart health.
Medications such as statins, ACE inhibitors, and antiplatelets play a crucial role in preventing heart attacks and managing related conditions. However, it’s important to discuss the benefits and potential risks or side effects with your healthcare provider to make informed decisions about your treatment plan.
Additionally, adopting a heart-healthy lifestyle is essential. Engaging in regular exercise, following a balanced diet, managing your weight, quitting smoking, moderating alcohol intake, and reducing stress levels all contribute to reducing the risk of heart attacks.
Key Takeaways:
- Preventing heart attacks is essential for maintaining heart health.
- Choosing the right medication can significantly lower the risk of heart attacks.
- Following preventive measures and treatment is crucial for reducing the chances of a heart attack.
Q: What are some common heart medications?
A: Some common heart medications include antiplatelet drugs, such as clopidogrel, and angiotensin-converting enzyme inhibitors to lower blood pressure and prevent blood clots.
Q: How do heart medications help treat heart conditions?
A: Heart medications help lower blood pressure and prevent blood clots, thus treating heart conditions such as heart failure, coronary artery disease, and preventing another heart attack.
Q: What are the risk factors for heart conditions that can be treated with medications?
A: Risk factors for heart conditions that can be treated with medications include high LDL cholesterol, heart muscle damage, and a history of heart attacks or heart failure.
Q: What are the types of heart medications used to prevent blood clots?
A: Antiplatelet drugs are a type of medication used to prevent blood clots that can lead to a heart attack. They are often prescribed following a heart attack or coronary artery bypass graft surgery.
Q: How do angiotensin-converting enzyme inhibitors work to treat heart conditions?
A: Angiotensin-converting enzyme inhibitors widen blood vessels, lower blood pressure, and improve blood flow to the heart, helping to treat heart conditions such as heart failure and prevent further heart muscle damage.
Q: What are some of the common side effects of heart medications?
A: Common side effects of heart medications may include changes in heart rate and blood pressure, as well as the risk of bleeding. However, it is essential to discuss the risks and benefits with your healthcare provider.
Q: How can heart medications help in preventing heart attacks?
A: Heart medications can help prevent heart attacks by lowering the risk of blood clot formation, reducing LDL cholesterol levels, and improving blood and oxygen supply to the heart muscle to reduce the risk of another heart attack.
Q: Are there specific guidelines for using heart medications from the American Heart Association?
A: Yes, the American Heart Association provides guidelines for the use of heart medications, and it is essential to follow these guidelines to ensure the most effective and safe treatment for heart conditions.
Q: How long do people typically need to take heart medications?
A: Many people may need to take heart medications for the rest of their lives to manage their heart conditions, prevent future heart events, and help maintain overall heart and blood vessel health.
Q: Can I stop taking my heart medications without consulting my healthcare provider?
A: It is important not to stop taking heart medications without consulting your healthcare provider, as discontinuing medication abruptly can lead to serious side effects and risks to your heart and overall health.
Q: What are the most common types of heart medications?
A: The most common types of heart medications include antiplatelet drugs, beta-blockers, ACE inhibitors, and statins, among others.
Q: How do heart medications help in preventing heart attacks?
A: Heart medications such as antiplatelet drugs and statins help in preventing heart attacks by reducing the risk of blood clots and lowering cholesterol levels.
Q: What is the role of heart medications in treating heart failure?
A: Heart medications help in treating heart failure by improving the heart’s ability to pump blood, reducing its workload, and managing symptoms such as shortness of breath and fatigue.
Q: Can heart medications lower blood pressure?
A: Yes, certain types of heart medications, such as ACE inhibitors and beta-blockers, can effectively lower blood pressure, thereby reducing the strain on the heart.
Q: What are the American Heart Association guidelines for the use of heart medications?
A: The American Heart Association provides guidelines for the use of heart medications based on the latest research and clinical trials to ensure the best possible treatment outcomes for heart patients.
Q: Are there specific medications used to treat heart attacks?
A: Yes, medications such as clopidogrel, aspirin, and thrombolytics are commonly used to treat heart attacks and restore blood flow to the heart.
Q: How do heart medications help in lowering LDL cholesterol?
A: Heart medications such as statins work by lowering LDL cholesterol levels, which helps reduce the risk of plaque buildup in the arteries and lowers the risk of heart disease.
Q: What role do heart medications play in preventing damage to the heart during a heart attack?
A: Heart medications help in preventing damage to the heart during a heart attack by improving blood flow, reducing the workload on the heart, and protecting against further complications.
Q: Can heart medications help improve blood flow and oxygen supply to the heart?
A: Yes, certain heart medications help improve blood flow and oxygen supply to the heart, which is essential for maintaining heart function and reducing the risk of cardiovascular events.
Q: What is the significance of diagnosing and treating heart rhythm disorders with specific types of heart medications?
A: Diagnosing and treating heart rhythm disorders with specific types of heart medications is crucial for maintaining a healthy heart rhythm and reducing the risk of cardiac complications.
Q: What are common heart medications used for heart attack treatment?
A: Common heart medications for heart attack treatment include antiplatelet drugs like clopidogrel, which help to prevent blood clots and improve blood flow to the heart.
Q: How do heart medications help the heart work better?
A: Heart medications help the heart work better by improving blood flow and oxygen delivery to the heart, which can reduce the workload on the heart and improve its overall function.
Q: What is the role of heart medications in preventing heart attacks?
A: Heart medications play a crucial role in preventing heart attacks by reducing the risk of blood clots and improving the blood supply to the heart, thus lowering the risk of having a heart attack.
Q: What are the American Heart Association guidelines for prescribing heart medications?
A: The American Heart Association provides guidelines for prescribing various types of heart medications to ensure optimal treatment and prevention of heart diseases. These guidelines are developed by expert editorial staff and reviewed by leading cardiologists and healthcare professionals.
Q: How are heart medications used in the treatment of congestive heart failure?
A: Heart medications are used in the treatment of congestive heart failure to help improve heart function and reduce symptoms, such as difficulty breathing and fluid retention. These medications can help your heart work better and improve your quality of life.
Q: What is the significance of heart medications in reducing the risk of myocardial infarction?
A: Heart medications are significant in reducing the risk of myocardial infarction, commonly known as a heart attack, by improving blood flow and reducing the workload on the heart, thus lowering the risk of having a heart attack.
Q: What type of medication is commonly prescribed to improve blood flow to the heart?
A: Antiplatelet drugs, such as clopidogrel, are commonly prescribed to improve blood flow to the heart and prevent blood clots, reducing the risk of heart attack and other cardiovascular events.
Q: How do heart medications impact the pumping function of the heart?
A: Heart medications can positively impact the pumping function of the heart by reducing the workload on the heart while ensuring adequate blood supply, thus helping the heart pump more effectively.
Q: What is the role of heart medications in the management of diagnosed heart conditions?
A: Heart medications play a crucial role in the management of diagnosed heart conditions by improving heart function and reducing symptoms, thus helping individuals with heart conditions live healthier and more active lives.
Q: How are heart medications recommended by the American College of Cardiology and the American Heart Association?
A: Heart medications are recommended by the American College of Cardiology and the American Heart Association based on evidence-based practices and extensive clinical research to provide the best possible care and treatment for individuals at risk of heart diseases in the U.S.
